Frailty is a clinical state of increased vulnerability due to age-associated decline in physiological reserve, resulting in compromised ability to cope with external everyday or acute stressors. (1) Preoperative frailty is associated with increased postoperative complications, mortality, and longer-term negative outcomes, including falls, lower quality of life, non-home discharge, and prolonged length of stay. (2,3)
Screening Tools
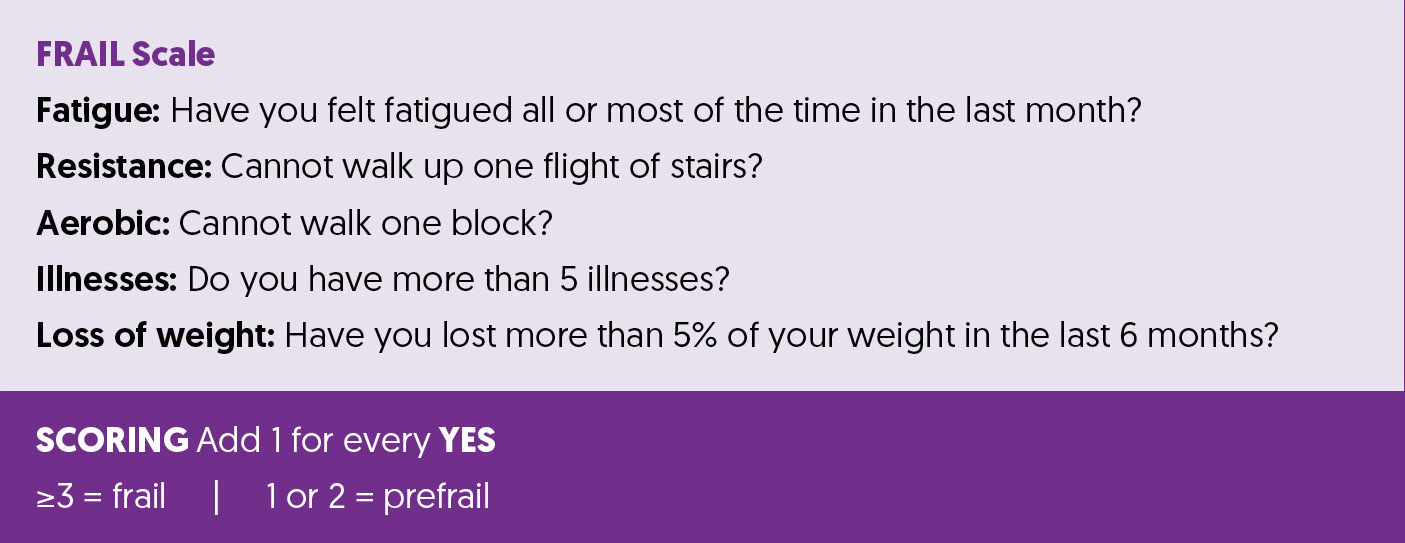
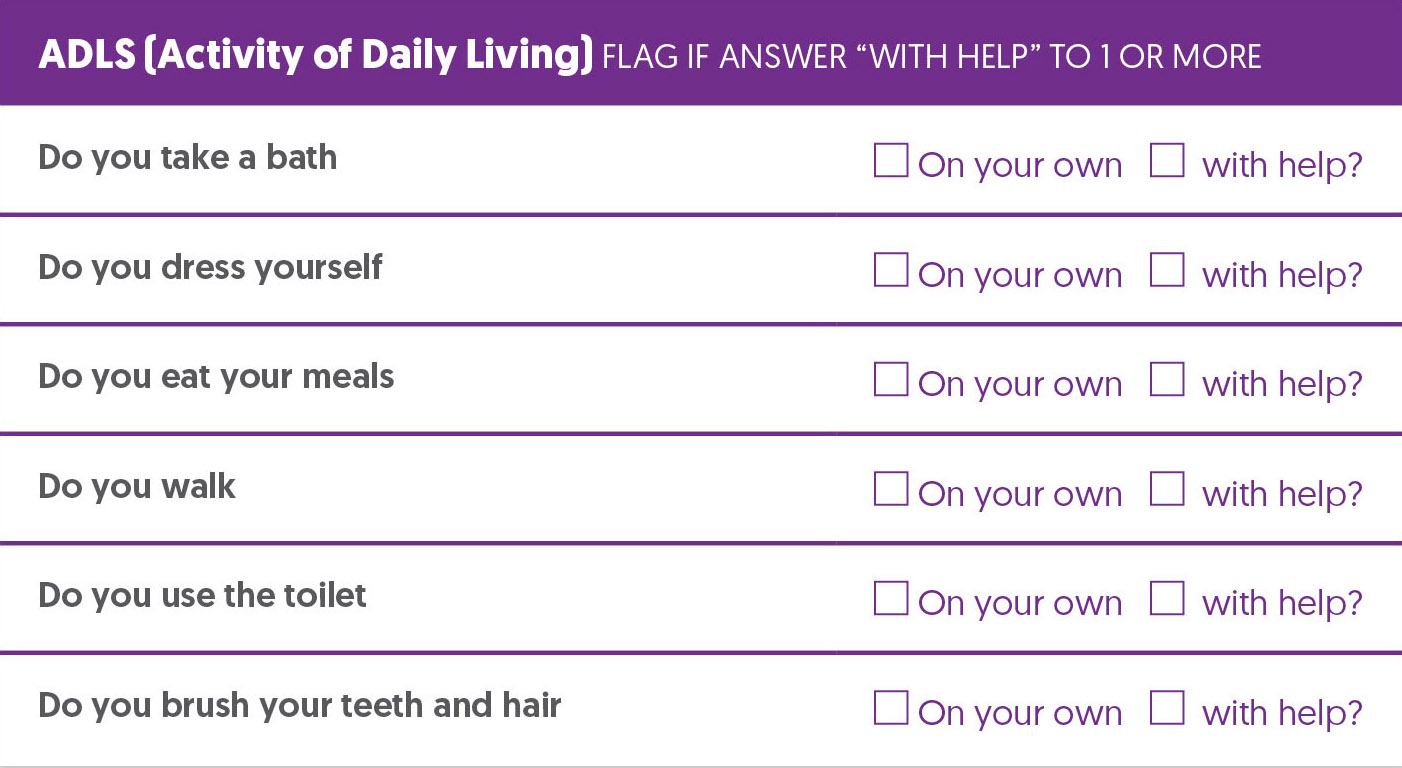
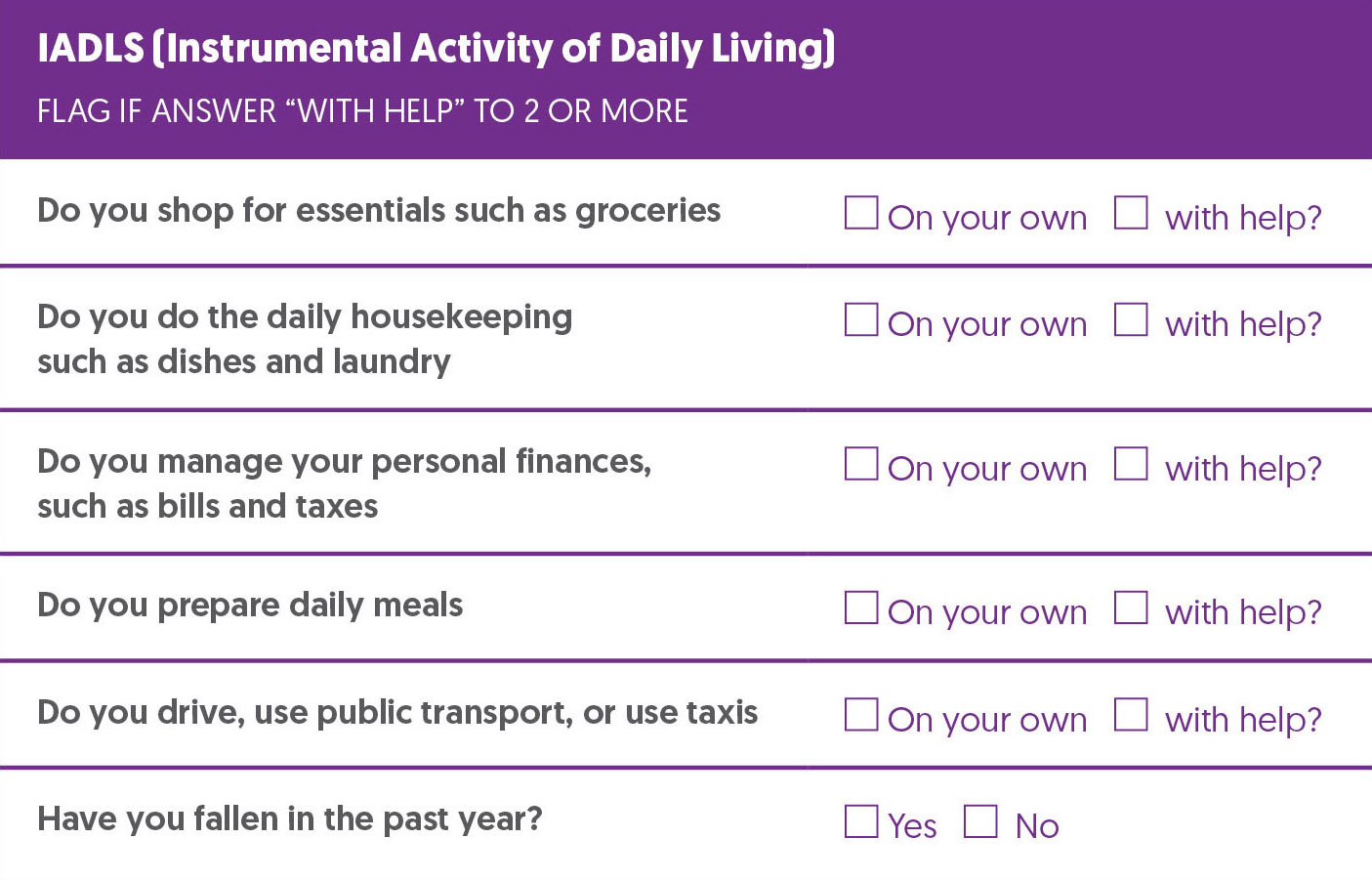
The FRAIL scale has been validated as a preoperative screening tool for frailty and as a predictor of mortality and postoperative complication. (4) Many geriatricians find ADLs and IADLs as a useful adjunct to a screening tool.
Prehabilitation and Optimization Algorithm
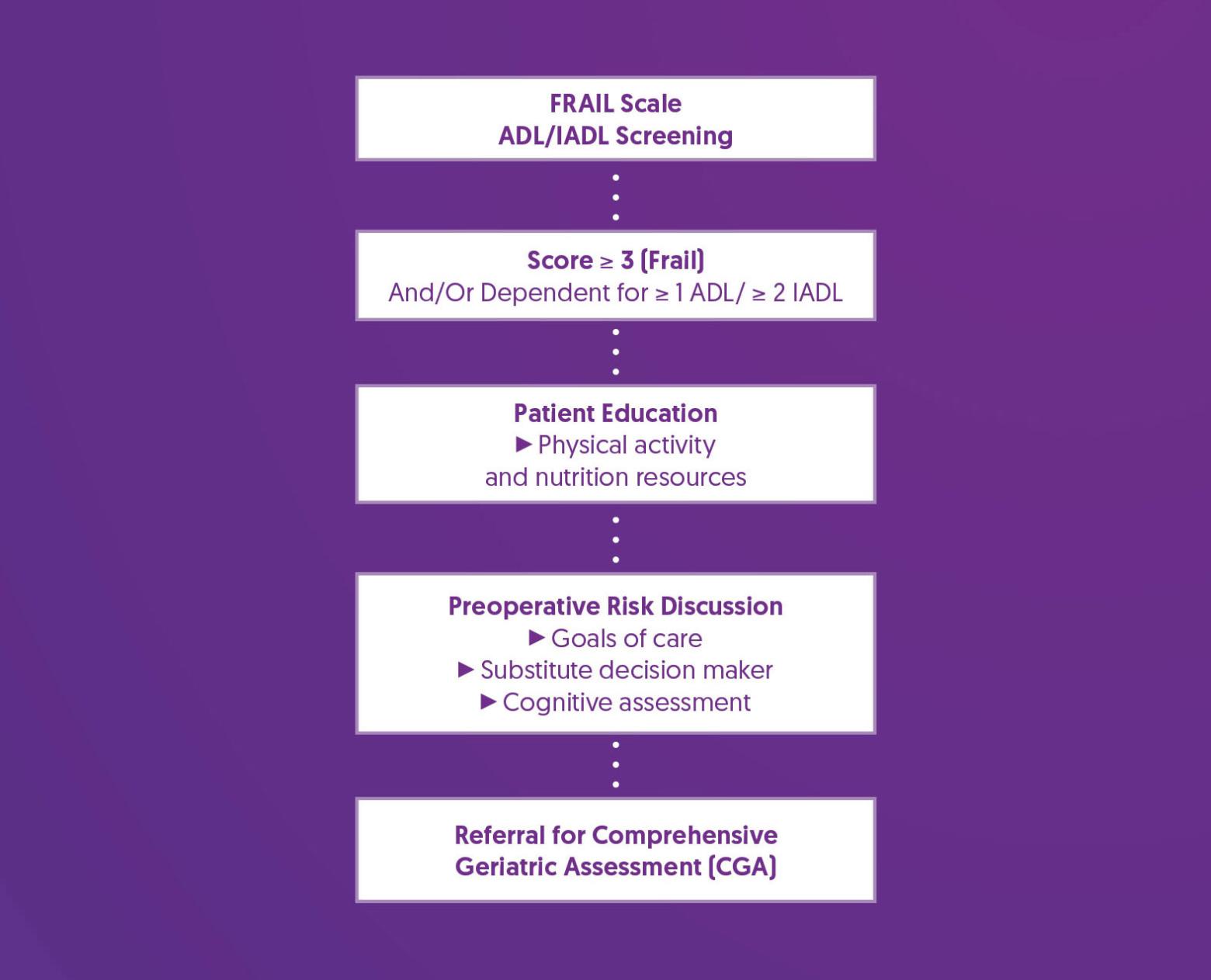
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Preoperative Risk Discussion |
|
| Referral for Comprehensive Geriatric Assessment (CGA) |
|
References
1. Fried, L. P., Tangen, C. M., Walston, J., Newman, A. B., Hirsch, C., Gottdiener, J., Seeman, T., Tracy, R., Kop, W. J., Burke, G., McBurnie, M. A., & Cardiovascular Health Study Collaborative Research Group (2001). Frailty in older adults: evidence for a phenotype. The journals of gerontology. Series A, Biological sciences and medical sciences, 56(3), M146–M156. https://doi.org/10.1093/gerona/56.3.m146
2. Lin, H. S., Watts, J. N., Peel, N. M., & Hubbard, R. E. (2016). Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC geriatrics, 16(1), 157. https://doi.org/10.1186/s12877-016-0329-8
3. McIsaac, D. I., Aucoin, S. D., Bryson, G. L., Hamilton, G. M., & Lalu, M. M. (2021). Complications as a Mediator of the Perioperative Frailty–Mortality Association. Anesthesiology, 134(4), 577–587. https://doi.org/10.1097/ALN.0000000000003699
4. Gong, S., Qian, D., Riazi, S., Chung, F., Englesakis, M., Li, Q., Huszti, E., & Wong, J. (2023). Association Between the FRAIL Scale and Postoperative Complications in Older Surgical Patients: A Systematic Review and Meta-Analysis. Anesthesia and analgesia, 136(2), 251–261. https://doi.org/10.1213/ANE.0000000000006272