Cannabis (marijuana) use may lead to increased anesthetic requirements, postoperative pain, opioid use after surgery, and nausea and vomiting. (1-3) Smoking cannabis increases the risk of pulmonary complications, cardiovascular complications (including postoperative myocardial infarction), and in-hospital mortality; it may also increase airway irritation, carboxyhemoglobin, and reduce oxygen-carrying capacity, similar to conventional cigarette smoking. (3-5)
Screening Tools
Cannabis Screening Questions:
Do you use Cannabis? If Yes:
- How often?
- How much do you use?
- How are you using it? (e.g., smoking, vaping, tincture/oil, edibles, cream)
- Have you ever had symptoms like headaches, anxiety, poor sleep, or stomach pain when you stopped using cannabis for a day or two (Cannabis Withdrawal Syndrome)?
Prehabilitation and Optimization Algorithm
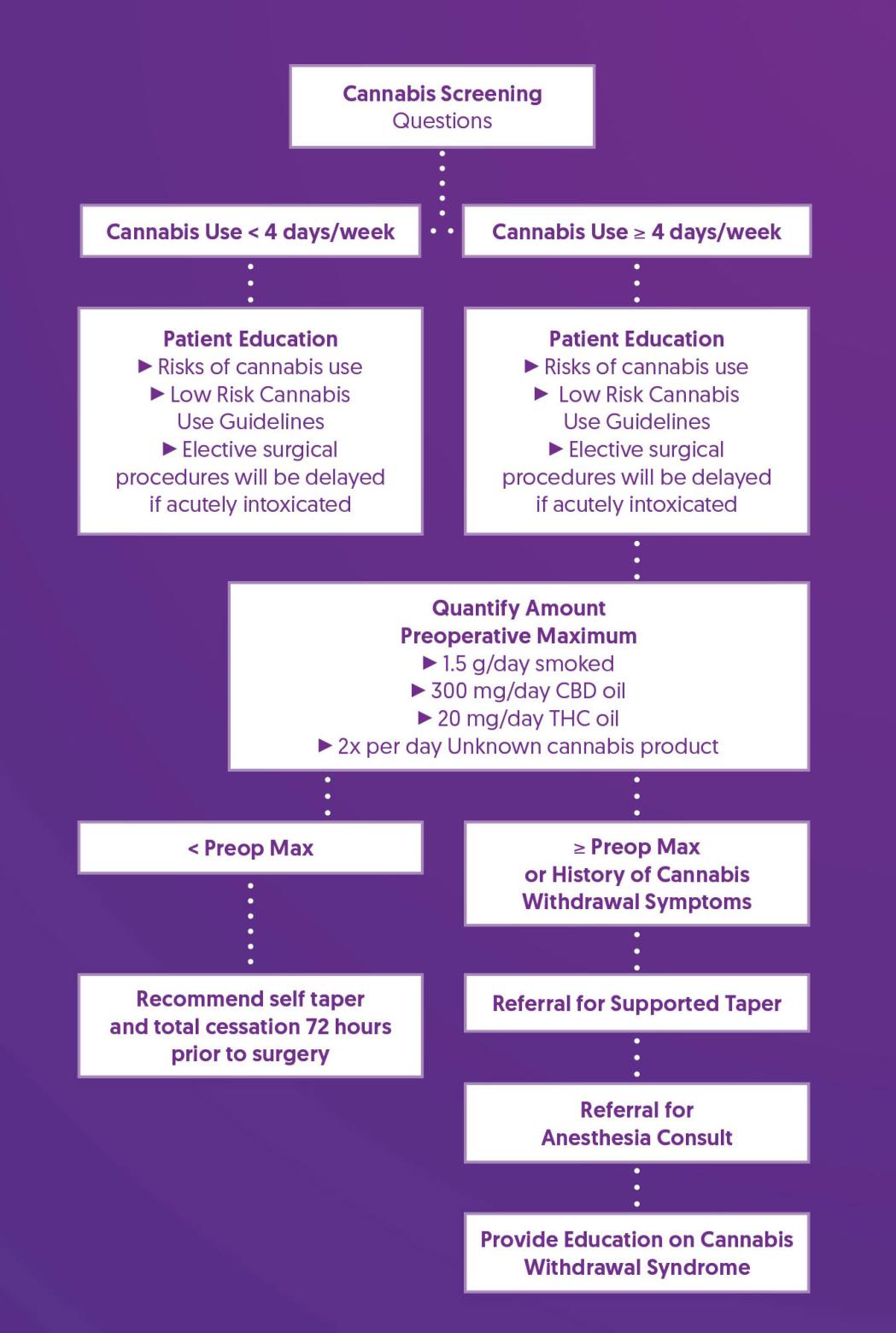
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Recommend Self Taper |
|
| Referral for Supported Taper |
|
| Referral for Anesthesia Consult |
|
| Provide Education on Cannabis Withdrawal Syndrome |
|
References
1. Ladha, K. S., McLaren-Blades, A., Goel, A., Buys, M. J., Farquhar-Smith, P., Haroutounian, S., Kotteeswaran, Y., Kwofie, K., Le Foll, B., Lightfoot, N. J., Loiselle, J., Mace, H., Nicholls, J., Regev, A., Rosseland, L. A., Shanthanna, H., Sinha, A., Sutherland, A., Tanguay, R., Yafai, S., … Clarke, H. (2021). Perioperative Pain and Addiction Interdisciplinary Network (PAIN): consensus recommendations for perioperative management of cannabis and cannabinoid-based medicine users by a modified Delphi process. British journal of anaesthesia, 126(1), 304–318. https://doi.org/10.1016/j.bja.2020.09.026
2. Shah, S., Schwenk, E. S., Sondekoppam, R. V., Clarke, H., Zakowski, M., Rzasa-Lynn, R. S., Yeung, B., Nicholson, K., Schwartz, G., Hooten, W. M., Wallace, M., Viscusi, E. R., & Narouze, S. (2023). ASRA Pain Medicine consensus guidelines on the management of the perioperative patient on cannabis and cannabinoids. Regional anesthesia and pain medicine, 48(3), 97–117. https://doi.org/10.1136/rapm-2022-104013
3. Echeverria-Villalobos, M., Todeschini, A. B., Stoicea, N., Fiorda-Diaz, J., Weaver, T., & Bergese, S. D. (2019). Perioperative care of cannabis users: A comprehensive review of pharmacological and anesthetic considerations. Journal of clinical anesthesia, 57, 41–49. https://doi.org/10.1016/j.jclinane.2019.03.011
4. Tetrault, J. M., Crothers, K., Moore, B. A., Mehra, R., Concato, J., & Fiellin, D. A. (2007). Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Archives of internal medicine, 167(3), 221–228. https://doi.org/10.1001/archinte.167.3.221
5. Jeffers, A. M., Glantz, S., Byers, A. L., & Keyhani, S. (2024). Association of Cannabis Use With Cardiovascular Outcomes Among US Adults. Journal of the American Heart Association, 13(5), e030178. https://doi.org/10.1161/JAHA.123.030178
6. The Centre for Addiction and Mental Health. (2017). 10 Ways to Reduce Risks to Your Health When Using Cannabis. https://www.camh.ca/-/media/files/pdfs---reports-and-books---research/canadas-lower-risk-guidelines-cannabis-pdf.pdf