In patients hospitalized for at least one night after non-cardiac surgery, the overall 30-day mortality rate is 1.8% with urgent/emergent surgery being associated with at lease double the risk of elective surgery. (1)
Many of these deaths are linked to cardiac complications (1). Myocardial Injury after Noncardiac Surgery (MINS), indicated by troponin levels exceeding the 99th percentile due to myocardial schema without ischemic features, occurs in 12-24% of cases (2). MINS is associated with a post-operative 30-day mortality rate of 9.8%, compared to 1% for those without it, and increases the risk of major vascular complications such as myocardial infarction and stroke (3,4,5).
Screening Tools
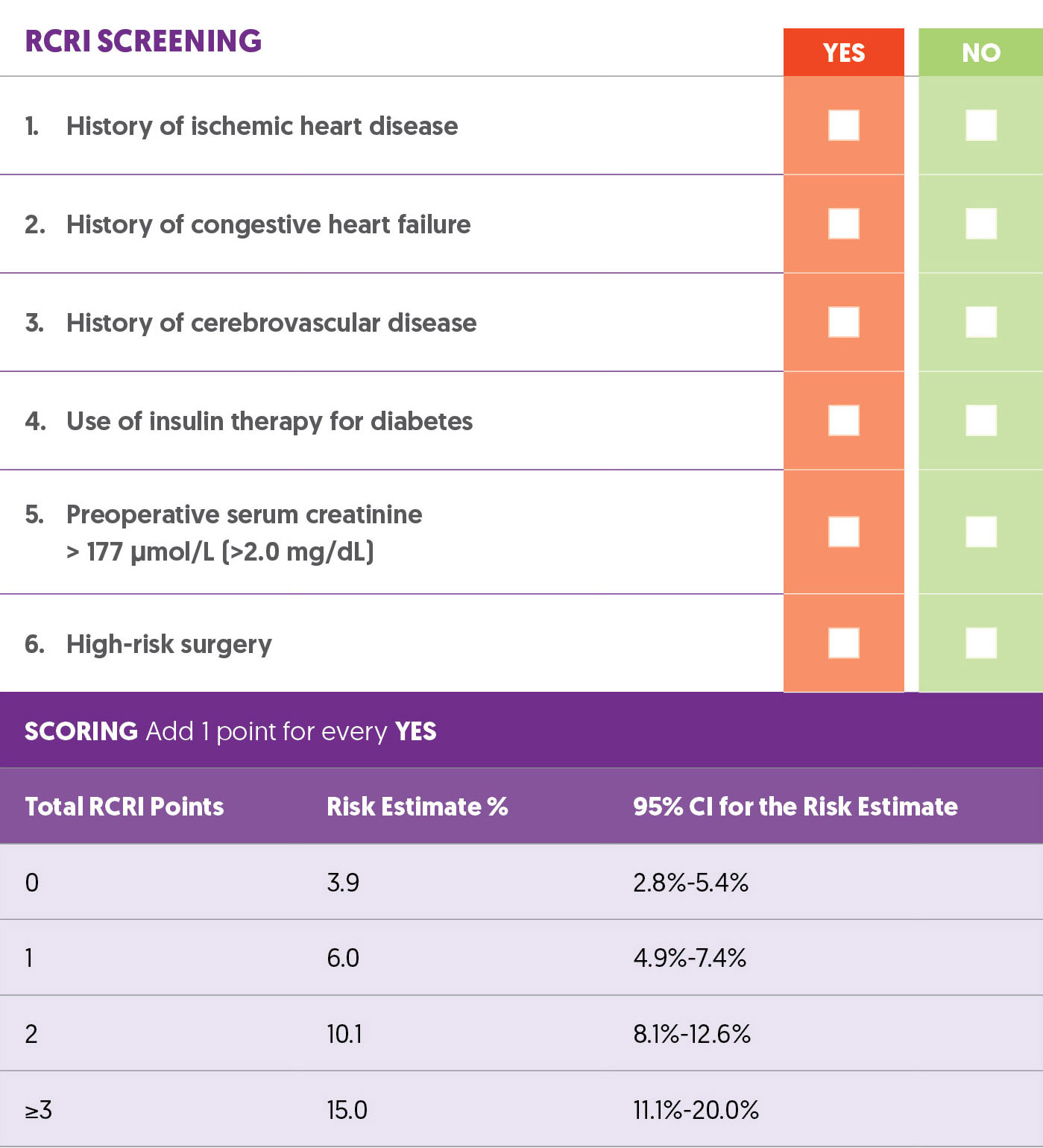
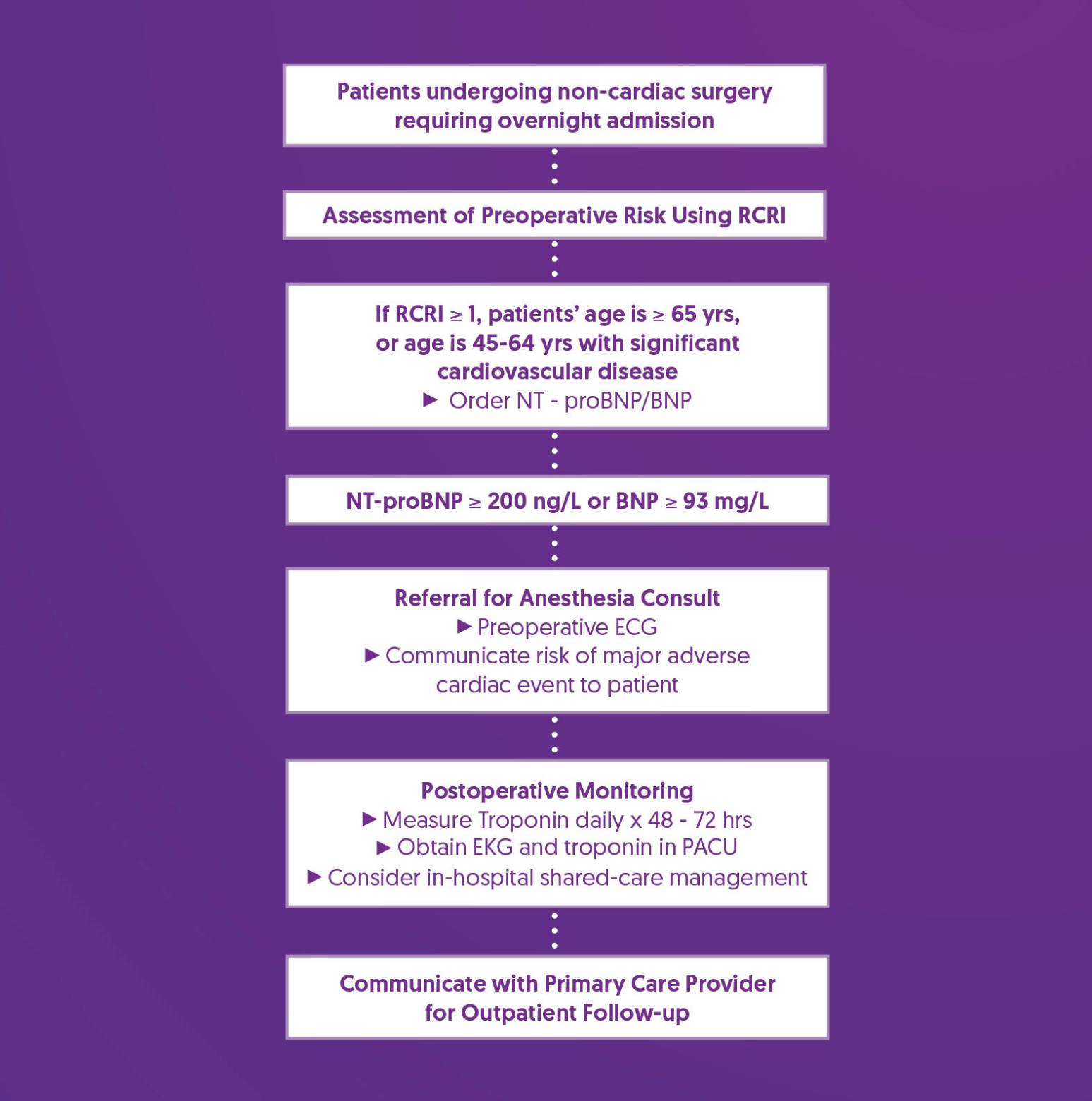
The Revised Cardiac Risk Index (RCRI) includes six factors, each worth 1 point (6). A review of 792,740 patients showed that the RCRI has moderate ability to predict major perioperative cardiac complications (7). For patients aged 65 or older, those aged 45-64 with significant cardiovascular disease, or those with an RCRI score ≥ 1, measure NT-proBNP or BNP before noncardiac surgery to improve risk assessment (8).
Revised Cardiac Risk Index (RCRI)
Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Order NT-proBNP/BNP |
|
| Referral for Anesthesia Consult |
|
| Postoperative Monitoring |
|
| Communicate with Primary Care Provider for Outpatient Follow-up |
|
References
1. Vascular Events in Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators, Spence, J., LeManach, Y., Chan, M. T. V., Wang, C. Y., Sigamani, A., Xavier, D., Pearse, R., Alonso-Coello, P., Garutti, I., Srinathan, S. K., Duceppe, E., Walsh, M., Borges, F. K., Malaga, G., Abraham, V., Faruqui, A., Berwanger, O., Biccard, B. M., Villar, J. C., … Devereaux, P. J. (2019). Association between complications and death within 30 days after noncardiac surgery. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 191(30), E830–E837. https://doi.org/10.1503/cmaj.190221
2. Smilowitz, N. R., Redel-Traub, G., Hausvater, A., Armanious, A., Nicholson, J., Puelacher, C., & Berger, J. S. (2019). Myocardial Injury After Noncardiac Surgery: A Systematic Review and Meta-Analysis. Cardiology in review, 27(6), 267–273. https://doi.org/10.1097/CRD.0000000000000254
3. Writing Committee for the VISION Study Investigators, Devereaux, P. J., Biccard, B. M., Sigamani, A., Xavier, D., Chan, M. T. V., Srinathan, S. K., Walsh, M., Abraham, V., Pearse, R., Wang, C. Y., Sessler, D. I., Kurz, A., Szczeklik, W., Berwanger, O., Villar, J. C., Malaga, G., Garg, A. X., Chow, C. K., Ackland, G., … Guyatt, G. H. (2017). Association of Postoperative High-Sensitivity Troponin Levels With Myocardial Injury and 30-Day Mortality Among Patients Undergoing Noncardiac Surgery. JAMA, 317(16), 1642–1651. https://doi.org/10.1001/jama.2017.4360
4. Devereaux, P. J., Duceppe, E., Guyatt, G., Tandon, V., Rodseth, R., Biccard, B. M., Xavier, D., Szczeklik, W., Meyhoff, C. S., Vincent, J., Franzosi, M. G., Srinathan, S. K., Erb, J., Magloire, P., Neary, J., Rao, M., Rahate, P. V., Chaudhry, N. K., Mayosi, B., de Nadal, M., … MANAGE Investigators (2018). Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet (London, England), 391(10137), 2325–2334. https://doi.org/10.1016/S0140-6736(18)30832-8
5. Botto, F., Alonso-Coello, P., Chan, M. T., Villar, J. C., Xavier, D., Srinathan, S., Guyatt, G., Cruz, P., Graham, M., Wang, C. Y., Berwanger, O., Pearse, R. M., Biccard, B. M., Abraham, V., Malaga, G., Hillis, G. S., Rodseth, R. N., Cook, D., Polanczyk, C. A., Szczeklik, W., … Vascular events In noncardiac Surgery patIents cOhort evaluatioN VISION Study Investigators (2014). Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology, 120(3), 564–578.https://doi.org/10.1097/ALN.0000000000000113
6. Lee, T. H., Marcantonio, E. R., Mangione, C. M., Thomas, E. J., Polanczyk, C. A., Cook, E. F., Sugarbaker, D. J., Donaldson, M. C., Poss, R., Ho, K. K., Ludwig, L. E., Pedan, A., & Goldman, L. (1999). Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation, 100(10), 1043–1049. https://doi.org/10.1161/01.cir.100.10.1043
7. Ford, M. K., Beattie, W. S., & Wijeysundera, D. N. (2010). Systematic review: prediction of perioperative cardiac complications and mortality by the revised cardiac risk index. Annals of internal medicine, 152(1), 26–35. https://doi.org/10.7326/0003-4819-152-1-201001050-00007
8. Duceppe, E., Parlow, J., MacDonald, P., Lyons, K., McMullen, M., Srinathan, S., Graham, M., Tandon, V., Styles, K., Bessissow, A., Sessler, D. I., Bryson, G., & Devereaux, P. J. (2017). Canadian Cardiovascular Society Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Noncardiac Surgery. The Canadian journal of cardiology, 33(1), 17–32. https://doi.org/10.1016/j.cjca.2016.09.008