Cigarette smoking is a risk factor for perioperative pulmonary, cardiovascular, bleeding and wound healing complications. (1,2) There is some evidence that vaping (or the use of e-cigarettes) is also associated with these complications. (3) The likelihood that quit-motivated patients can abstain from smoking is increased by use of nicotine replacement therapy (NRT). (4)
Screening Tools
Screening Questions:
- Do you currently use products that contain tobacco or nicotine? (e.g., smoking cigarettes or e-cigarettes, vaping nicotine, or chewing tobacco)
- If Yes, what type of tobacco/nicotine product?
- If cigarettes, how many packs/day? If other, how much & how often?
Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Patient Education |
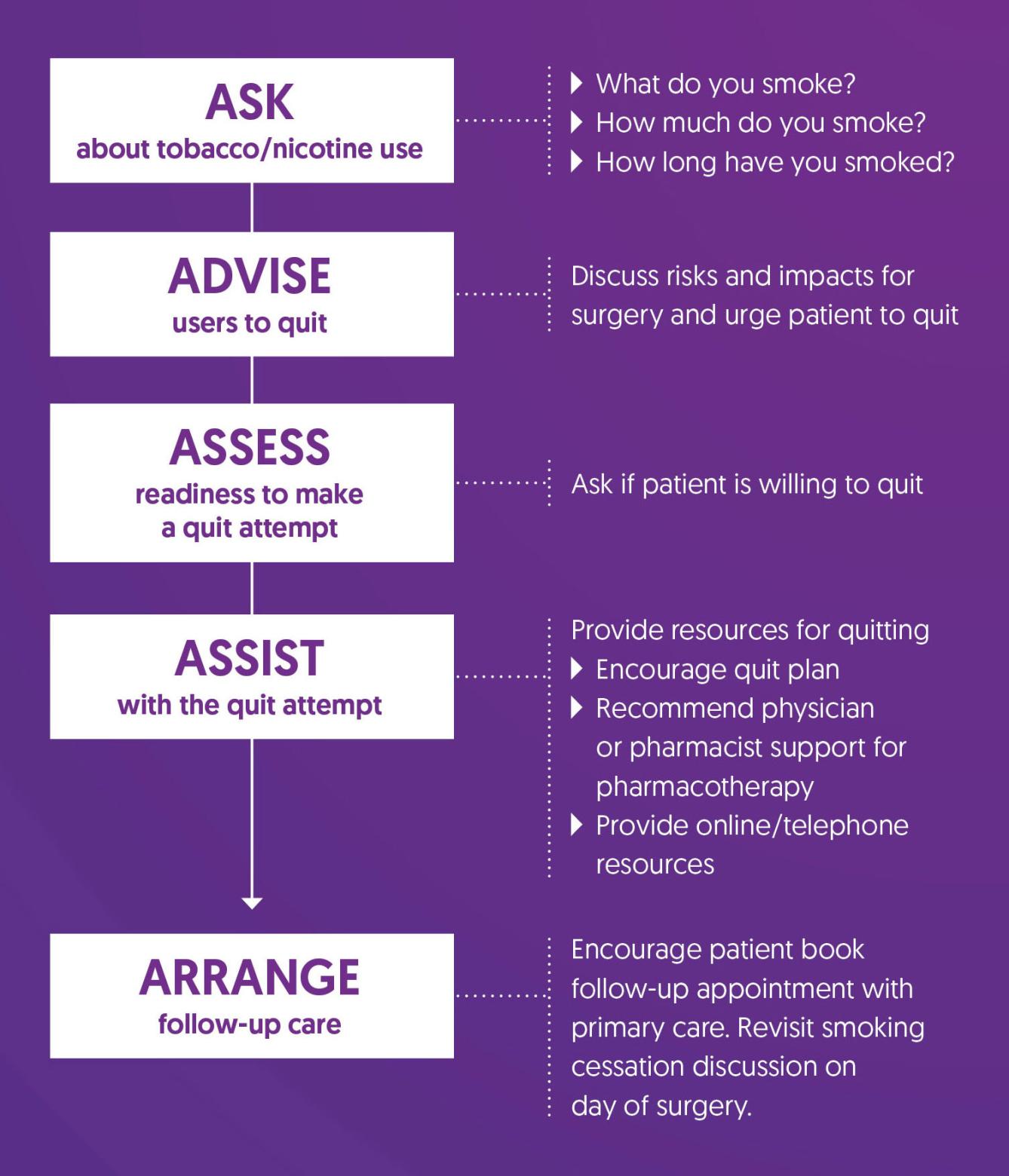
5 A’s Algorithm for Smoking Cessation (5).
|
| Referral for Follow-up |
|
References
1. Eliasen, M., Grønkjær, M., Skov-Ettrup, L. S., Mikkelsen, S. S., Becker, U., Tolstrup, J. S., & Flensborg-Madsen, T. (2013). Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Annals of surgery, 258(6), 930–942. https://doi.org/10.1097/SLA.0b013e3182988d59
2. Turan, A., Mascha, E., Roberman, D., Turner, P. L., You, J., Kurz, A., Sessler, D. I., Saager, L. (2011). Smoking and Perioperative Outcomes. Anesthesiology, 114(4), 837-846. https://doi.org/10.1098/ALN.0b013e318210f560
3. Rusy, D., Honkanen, A., Landrigan-Ossar, M. F., Chatterjee, D., Schwartz, L., Lalwani, K., Dollar, J., Clark, R., Diaz, C. D., Deutsch, N., Warner, D. O., Soriano, S. G., (2021). Vaping and E-Cigarette Use in Children and Adolescents: Implications on Perioperative Care from the American Society of Anesthesiologists Committee on Pediatric Anesthesia, Society for Pediatric Anesthesia, and American Academy of Pediatrics Section on Anesthesiology and Pain Medicine. Anesthesia & Analgesia, 133(3), 562-568. https://doi.org/10.1213/ANE.0000000000005519
4. Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of internal medicine, 158(16), 1789–1795. https://doi.org/10.1001/archinte.158.16.1789
5. Fiore, M. C., Jaén, C. R., Baker, T. B., et al. (2008). Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. U.S. Department of Health and Human Services, Public Health Service. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians/update/treating_tobacco_use08.pdf
6. Government of British Columbia (n.d.). Smoking Cessation Program – information for health professionals. Retrieved October 18, 2024, from https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/pharmacies/smoking-cessation-program-for-health-professionals