Preoperative anemia is common, especially in orthopedic, gynecologic, and colorectal surgical patients. (1,2) “The presence of preoperative anemia, even if mild, has been associated with increased risk of red blood cell (RBC) transfusion and increased morbidity and mortality after surgery. In addition, transfusion of RBCs has been consistently associated with worsened clinical outcomes”. (3)
Screening Tools
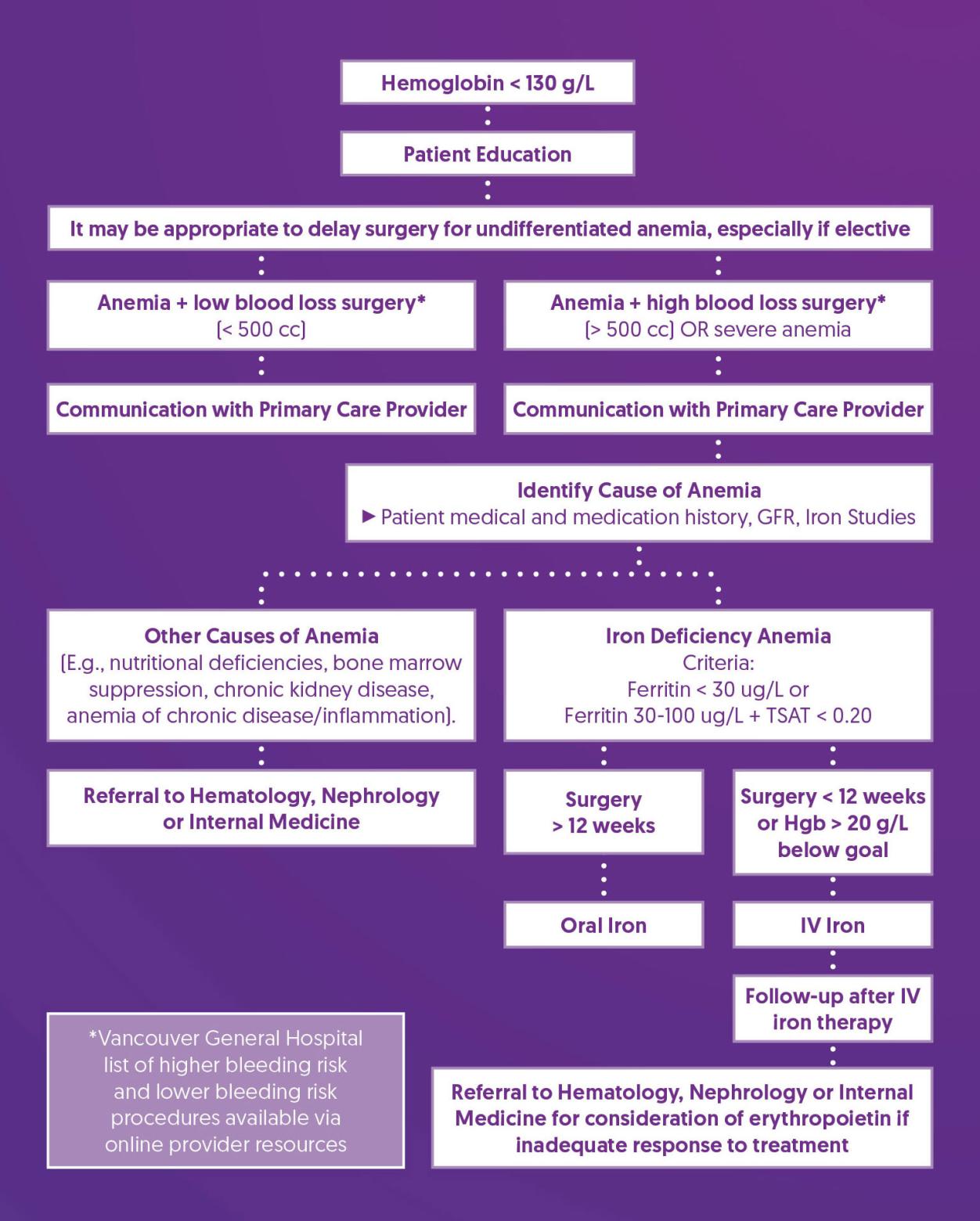
Preoperative hemoglobin (Hgb) is recommended for screening based on patient co-morbidities and surgical invasiveness, as per site specific protocols. (3) If a patient is found to be anemic, basic screening for iron deficiency anemia as well as other causes (e.g., chronic kidney disease) is recommended.
Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Consider Delaying Surgery |
|
| Communication with Primary Care Provider |
|
| Identify Cause of Anemia |
|
| Treat Iron Deficiency Anemia |
|
| Follow-up After IV Iron Therapy |
|
| Referral to Hematology, Nephrology, or Internal Medicine |
|
References
1. Muñoz, M., Laso-Morales, M. J., Gómez-Ramírez, S., Cadellas, M., Núñez-Matas, M. J., & García-Erce, J. A. (2017). Pre-operative haemoglobin levels and iron status in a large multicentre cohort of patients undergoing major elective surgery. Anaesthesia, 72(7), 826–834. https://doi.org/10.1111/anae.13840
2. Baron, D. M., Hochrieser, H., Posch, M., Metnitz, B., Rhodes, A., Moreno, R. P., Pearse, R. M., Metnitz, P., European Surgical Outcomes Study (EuSOS) group for Trials Groups of European Society of Intensive Care Medicine, & European Society of Anaesthesiology (2014). Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. British journal of anaesthesia, 113(3), 416–423. https://doi.org/10.1093/bja/aeu098
3. Shander, A., Corwin, H. L., Meier, J., Auerbach, M., Bisbe, E., Blitz, J., Erhard, J., Faraoni, D., Farmer, S. L., Frank, S. M., Girelli, D., Hall, T., Hardy, J. F., Hofmann, A., Lee, C. K., Leung, T. W., Ozawa, S., Sathar, J., Spahn, D. R., Torres, R., … Muñoz, M. (2023). Recommendations From the International Consensus Conference on Anemia Management in Surgical Patients (ICCAMS). Annals of surgery, 277(4), 581–590. https://doi.org/10.1097/SLA.0000000000005721
4. BCGuidelines.ca. Iron Deficiency – Diagnosis and Management (2019) Appendix A: Oral Iron Formulations and Adult Doses. https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/...