Preoperative anemia is common, especially in orthopedic, gynecologic, and colorectal surgical patients. (1,2) “The presence of preoperative anemia, even if mild, has been associated with increased risk of red blood cell (RBC) transfusion and increased morbidity and mortality after surgery. In addition, transfusion of RBCs has been consistently associated with worsened clinical outcomes”. (3)
Screening Tools
Preoperative hemoglobin (Hgb) is recommended for screening based on patient co-morbidities and surgical invasiveness, as per site specific protocols. (3) If a patient is found to be anemic, basic screening for iron deficiency anemia as well as other causes (e.g., chronic kidney disease) is recommended.
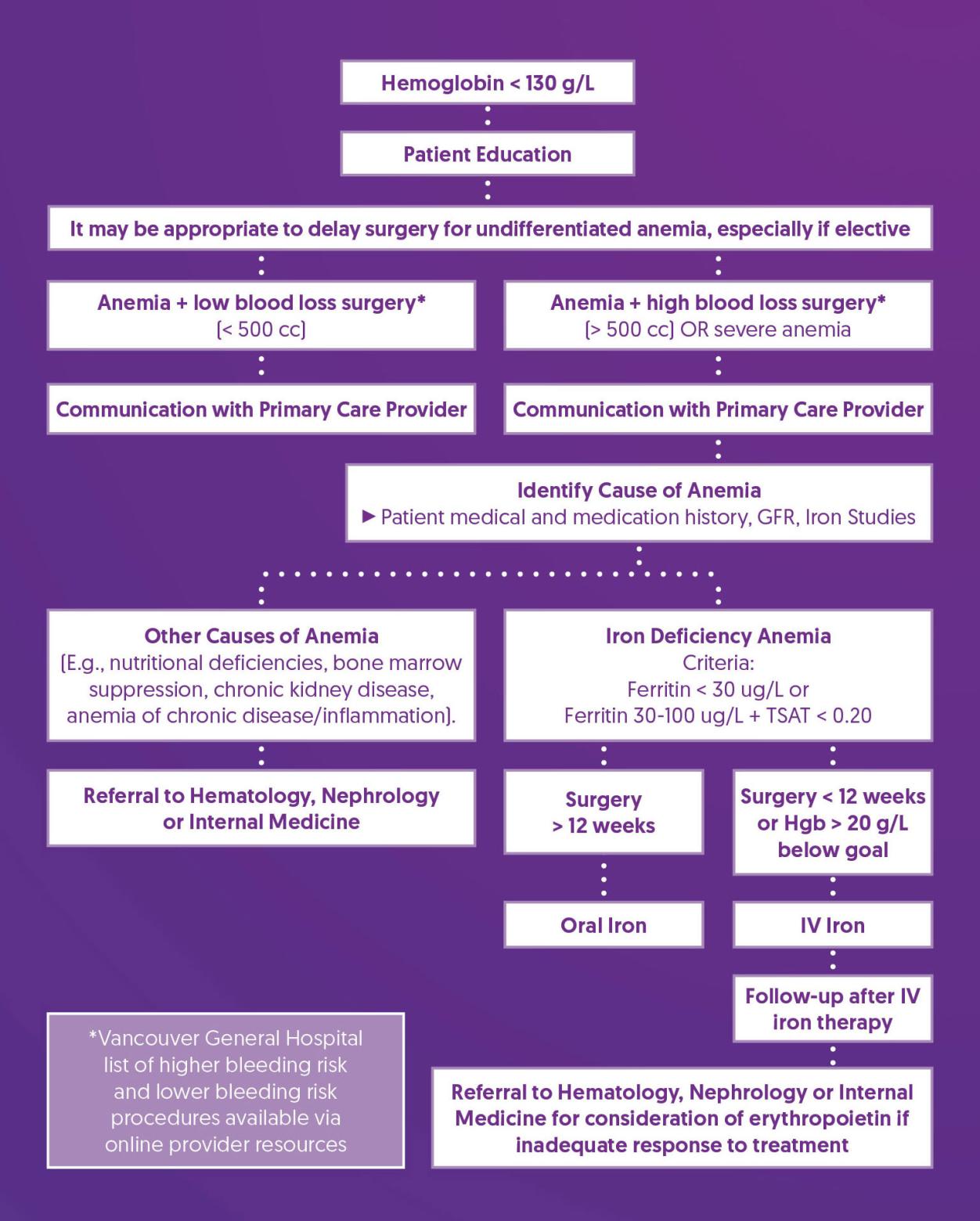
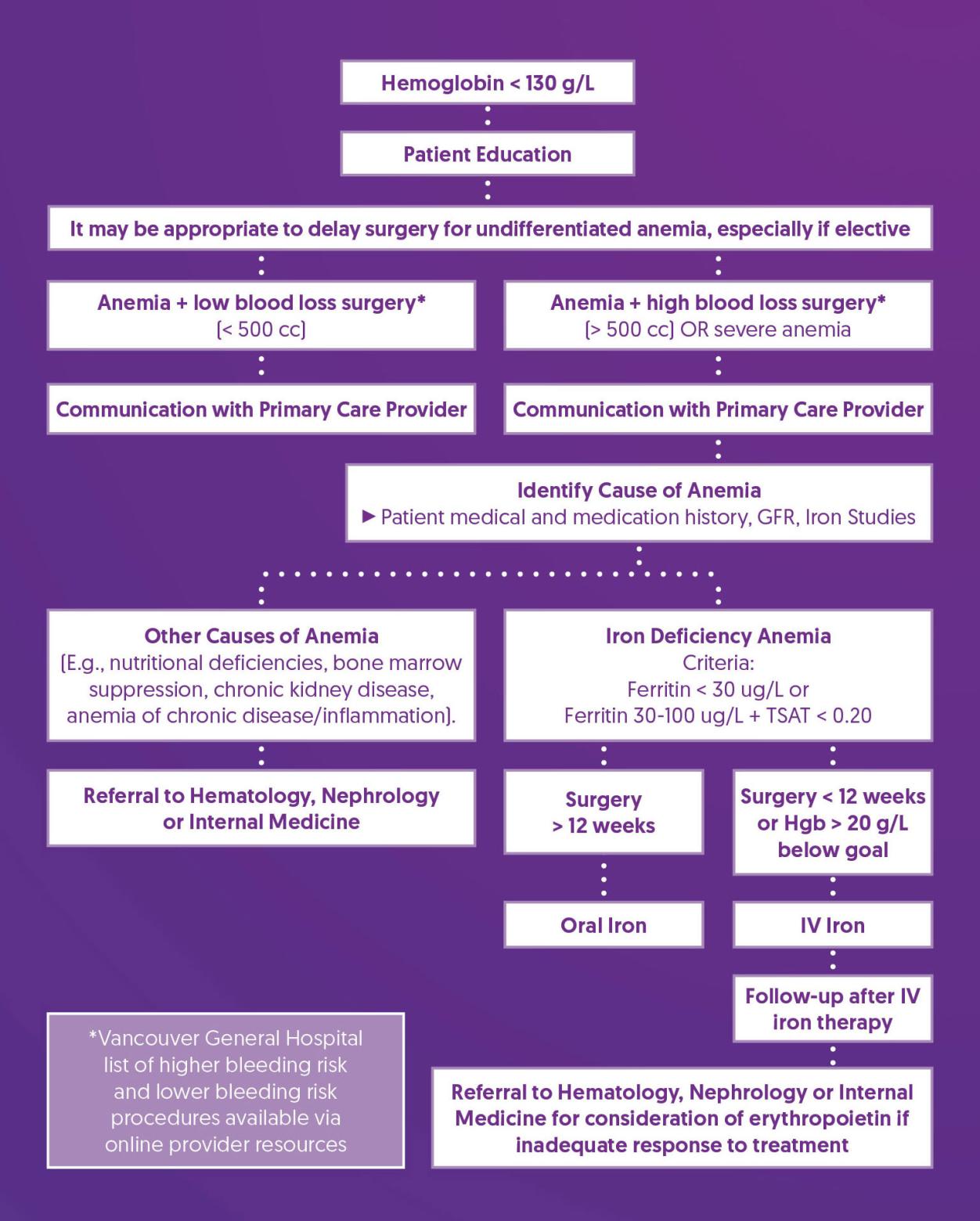
Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Patient Education |
- Communicate importance of optimizing hemoglobin before surgery to decrease perioperative risks
- Refer to online patient resources
|
| Consider Delaying Surgery |
- For cases of anemia with an unclear cause or iron deficiency anemia that is not related to the reason for surgery, consider postponing elective surgery to allow time for further investigation and treatment of the anemia to support better surgical outcomes and reduce potential complications. Suggest communication with surgical team.
- Patients undergoing high blood loss surgeries who would decline transfusion require special consideration. Consider multidisciplinary discussion and delaying surgery until hemoglobin goal is reached.
|
| Communication with Primary Care Provider |
- If a patient is found to have anemia before surgery and does not meet the criteria for perioperative optimization, it is important to inform the patient and request their primary care provider investigate and treat the underlying cause of the anemia. This is particularly crucial for patients with unexplained iron deficiency anemia, as they may need further evaluation to rule out serious conditions like gastrointestinal cancers.
|
| Identify Cause of Anemia |
- Population for optimization: surgeries with expected blood loss >= 500 mL or patients with severe anemia
- Example high blood loss surgeries include*: redo/bilateral joints, multilevel spine, open gynecology, open bowel resection/general surgery, major urology cases, all cardiac, open thoracics, radical prostatectomies
*full list of high and low blood loss surgeries for Vancouver General Hospital available via online provider resources
- Recommend performing basic screening to identify possible underlying causes of anemia. This should include taking a detailed bleeding history, reviewing the patient's medication history, and testing (e.g., iron studies, renal function)
|
| Treat Iron Deficiency Anemia |
- Criteria: Ferritin < 30 ng/L or Ferritin 30-100 ng/L and transferrin saturation < 0.20
- If surgery > 12 weeks away: oral iron (e.g., ferrous fumarate 300 mg PO every other night with 600-1200 mg vitamin C (4)); recheck Hgb after one month
- If surgery < 12 weeks away: IV iron dose can be based on the Ganzoni formula or standardized dosing (e.g., iron isomaltoside 1000 mg x 1 dose or iron sucrose 300 mg x 3 doses)
|
| Follow-up After IV Iron Therapy |
- IV iron takes 10-14 days for full effect, expect increase of up to 10 g/L/week
- Follow-up bloodwork should be arranged for 10-14 days post iron infusion and flagged for anesthesia review
- Ensure CBC is re-done within 30 days of surgical procedure
- After administering iron supplementation, the goal is to treat anemia so that hemoglobin levels reach above 130 g/L. If this target is not met before the scheduled surgery, clinical judgment should be used to decide whether to delay the surgery until the goal is achieve
- May recommend postoperative oral iron for patients having major surgery as it has been shown to speed recovery.
|
| Referral to Hematology, Nephrology, or Internal Medicine |
- If there are other potential causes of anemia besides iron deficiency (e.g., nutritional deficiencies, bone marrow suppression, chronic kidney disease, anemia of chronic disease/inflammation), or if the patient shows an inadequate response to iron treatment, consider referring the patient to a subspecialist.
|
References
1. Muñoz, M., Laso-Morales, M. J., Gómez-Ramírez, S., Cadellas, M., Núñez-Matas, M. J., & García-Erce, J. A. (2017). Pre-operative haemoglobin levels and iron status in a large multicentre cohort of patients undergoing major elective surgery. Anaesthesia, 72(7), 826–834. https://doi.org/10.1111/anae.13840
2. Baron, D. M., Hochrieser, H., Posch, M., Metnitz, B., Rhodes, A., Moreno, R. P., Pearse, R. M., Metnitz, P., European Surgical Outcomes Study (EuSOS) group for Trials Groups of European Society of Intensive Care Medicine, & European Society of Anaesthesiology (2014). Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. British journal of anaesthesia, 113(3), 416–423. https://doi.org/10.1093/bja/aeu098
3. Shander, A., Corwin, H. L., Meier, J., Auerbach, M., Bisbe, E., Blitz, J., Erhard, J., Faraoni, D., Farmer, S. L., Frank, S. M., Girelli, D., Hall, T., Hardy, J. F., Hofmann, A., Lee, C. K., Leung, T. W., Ozawa, S., Sathar, J., Spahn, D. R., Torres, R., … Muñoz, M. (2023). Recommendations From the International Consensus Conference on Anemia Management in Surgical Patients (ICCAMS). Annals of surgery, 277(4), 581–590. https://doi.org/10.1097/SLA.0000000000005721
4. BCGuidelines.ca. Iron Deficiency – Diagnosis and Management (2019) Appendix A: Oral Iron Formulations and Adult Doses. https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/...