Obstructive sleep apnea (OSA) is a chronic medical condition that is commonly undiagnosed. The most common form of sleep-disordered breathing, it is characterized by recurring transient obstructions of airflow that occur exclusively during sleep. OSA is associated with increased risk of perioperative complications, including postoperative respiratory failure, cardiac events, and ICU transfer, and should be identified and treated as early as possible to help reduce this risk. (1-7)
Screening Tools
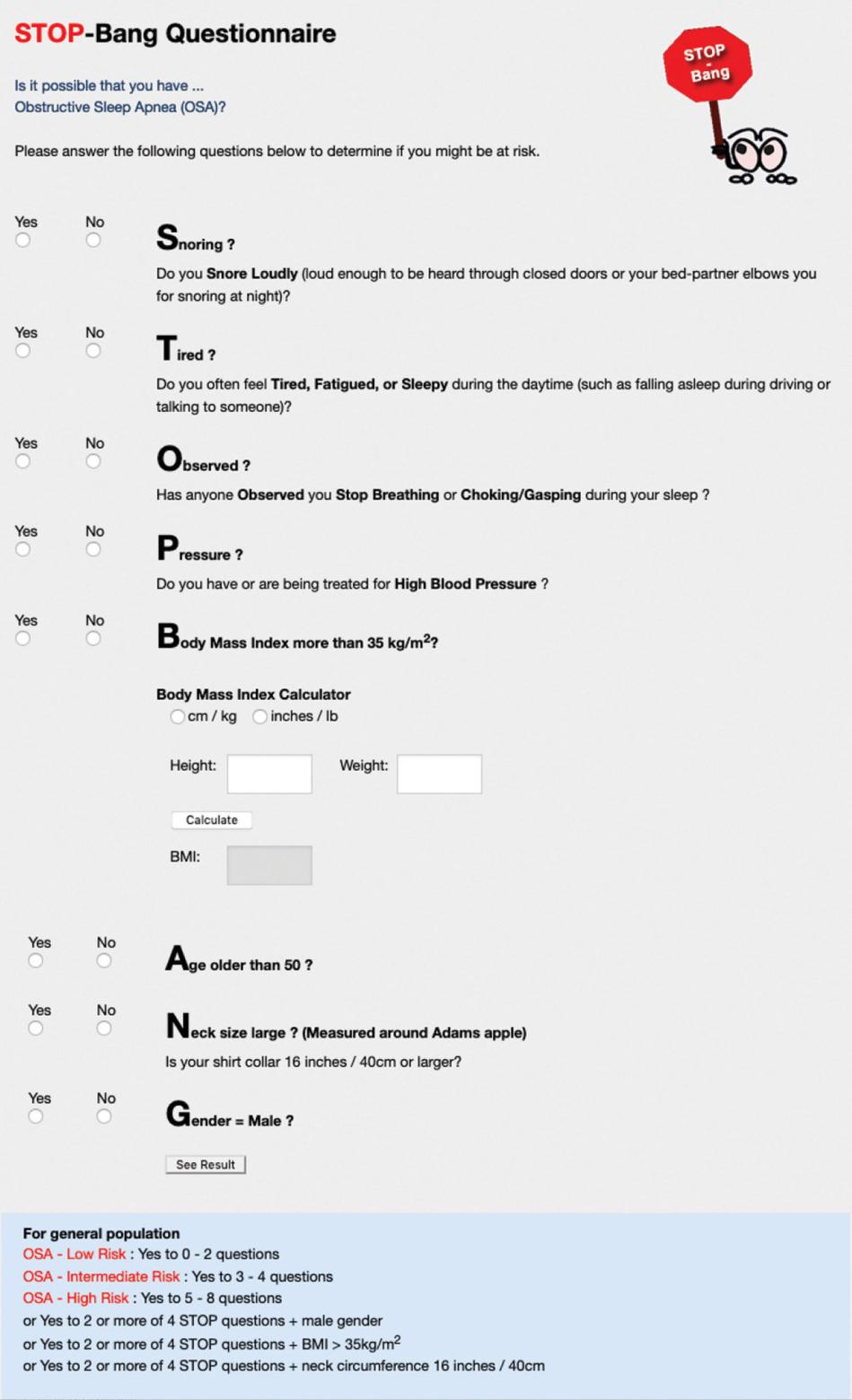
The STOP-Bang questionnaire is a validated tool for preoperative screening for OSA, assessing the likelihood of moderate to severe OSA. Scores of 5 or higher indicate a high probability of moderate to severe OSA. (8)
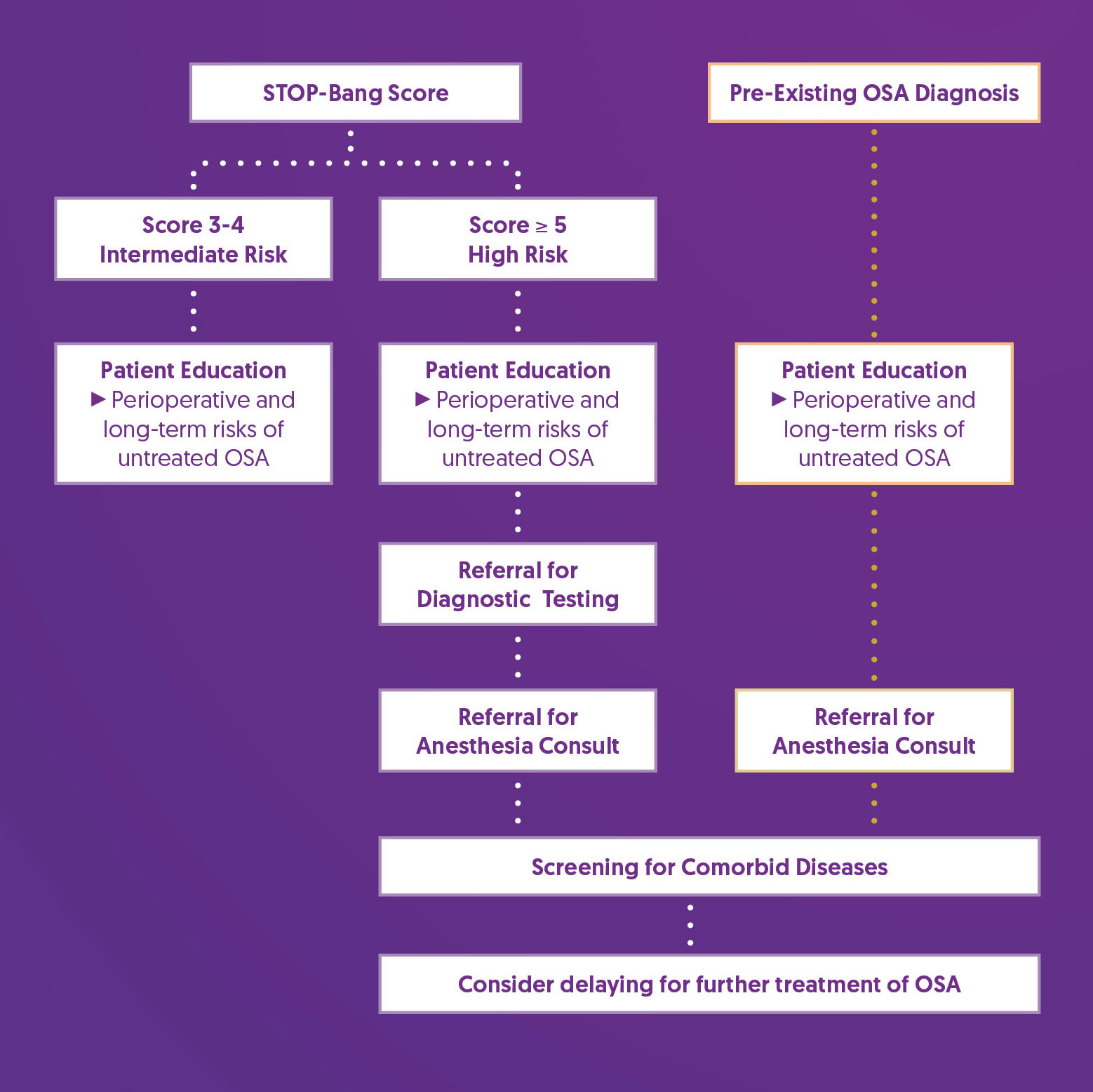
Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Referral for Diagnostic Testing |
|
| Referral for Anesthesia Consult |
|
| Screening for Comorbid Disease |
|
| Consider delaying for further treatment of OSA |
|
References
1. Roesslein, M., & Chung, F. (2018). Obstructive sleep apnoea in adults: peri-operative considerations: A narrative review. European journal of anaesthesiology, 35(4), 245–255. https://doi.org/10.1097/EJA.0000000000000765
2. Mutter, T. C., Chateau, D., Moffatt, M., Ramsey, C., Roos, L. L., & Kryger, M. (2014). A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology, 121(4), 707–718. https://doi.org/10.1097/ALN.0000000000000407
3. Abdelsattar, Z. M., Hendren, S., Wong, S. L., Campbell, D. A., Jr, & Ramachandran, S. K. (2015). The Impact of Untreated Obstructive Sleep Apnea on Cardiopulmonary Complications in General and Vascular Surgery: A Cohort Study. Sleep, 38(8), 1205–1210. https://doi.org/10.5665/sleep.4892
4. Patel, D., Tsang, J., Saripella, A., Nagappa, M., Islam, S., Englesakis, M., & Chung, F. (2022). Validation of the STOP questionnaire as a screening tool for OSA among different populations: a systematic review and meta-regression analysis. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 18(5), 1441–1453. https://doi.org/10.5664/jcsm.9820
5. Melesse, D. Y., Mekonnen, Z. A., Kassahun, H. G., & Chekol, W. B. (2020). Evidence based perioperative optimization of patients with obstructive sleep apnea in Resource Limited Areas: A systematic review. International Journal of Surgery Open, 23, 23–34. https://doi.org/10.1016/j.ijso.2020.02.002
6. Cozowicz, C., & Memtsoudis, S. G. (2021). Perioperative Management of the Patient With Obstructive Sleep Apnea: A Narrative Review. Anesthesia and analgesia, 132(5), 1231–1243. https://doi.org/10.1213/ANE.0000000000005444
7. Chaudhry, R. A., Zarmer, L., West, K., & Chung, F. (2024). Obstructive Sleep Apnea and Risk of Postoperative Complications after Non-Cardiac Surgery. Journal of clinical medicine, 13(9), 2538. https://doi.org/10.3390/jcm13092538
8. Hwang, M., Nagappa, M., Guluzade, N., Saripella, A., Englesakis, M., & Chung, F. (2022). Validation of the STOP-Bang questionnaire as a preoperative screening tool for obstructive sleep apnea: a systematic review and meta-analysis. BMC anesthesiology, 22(1), 366. https://doi.org/10.1186/s12871-022-01912-1
9. Chung, F., Memtsoudis, S. G., Ramachandran, S. K., Nagappa, M., Opperer, M., Cozowicz, C., Patrawala, S., Lam, D., Kumar, A., Joshi, G. P., Fleetham, J., Ayas, N., Collop, N., Doufas, A. G., Eikermann, M., Englesakis, M., Gali, B., Gay, P., Hernandez, A. V., Kaw, R., … Auckley, D. (2016). Society of Anesthesia and Sleep Medicine Guidelines on Preoperative Screening and Assessment of Adult Patients With Obstructive Sleep Apnea. Anesthesia and analgesia, 123(2), 452–473. https://doi.org/10.1213/ANE.0000000000001416