Postoperative delirium is one of the most common complications following major surgery. While many cases may be preventable, it may affect up to half of older adults and often goes unrecognized. It is associated with increased postoperative complications, length of stay in hospital, non-home discharge, mortality, and healthcare costs, as well as decline in function and cognition. (1-4)
Screening Tools
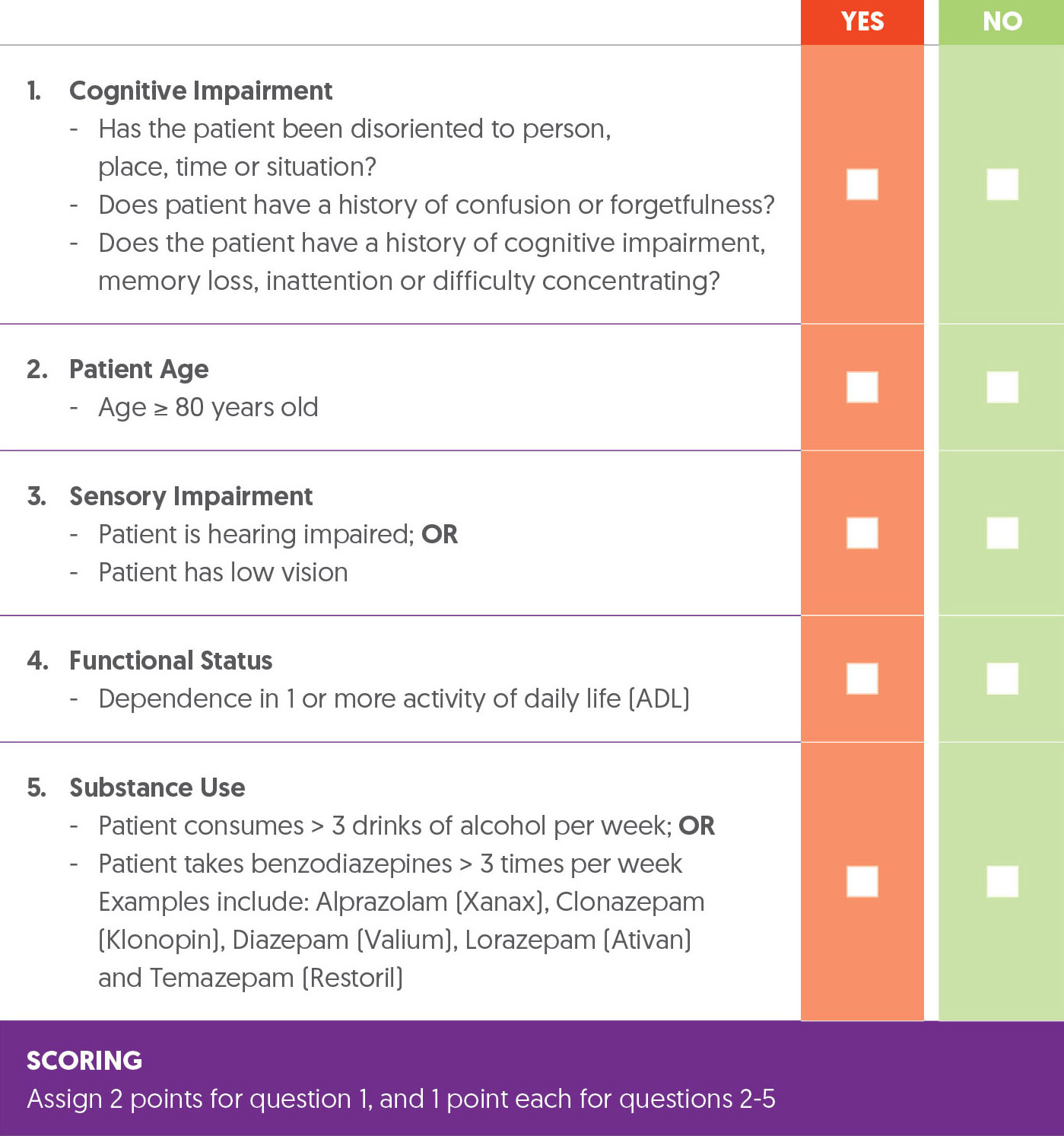
The Delirium Elderly At-Risk (DEAR) instrument has been used to predict postoperative delirium in elective and emergency orthopedic patients based on cognitive impairment, age, functional dependence, sensory impairment, and chronic substance use. “Among arthroplasty patients, having two or more risk factors was associated with an eight-fold increase in the incidence of delirium.” (1) The modified DEAR (mDEAR) uses routinely collected medical record data to assess cognitive impairment instead of the MMSE utilized in the DEAR and attributes 2 points to cognitive impairment and 1 point to each other factor. A patient scoring 3 or more indicates a higher risk of developing delirium. (5)
mDEAR Screening Instrument
Prehabilitation and Optimization Algorithm
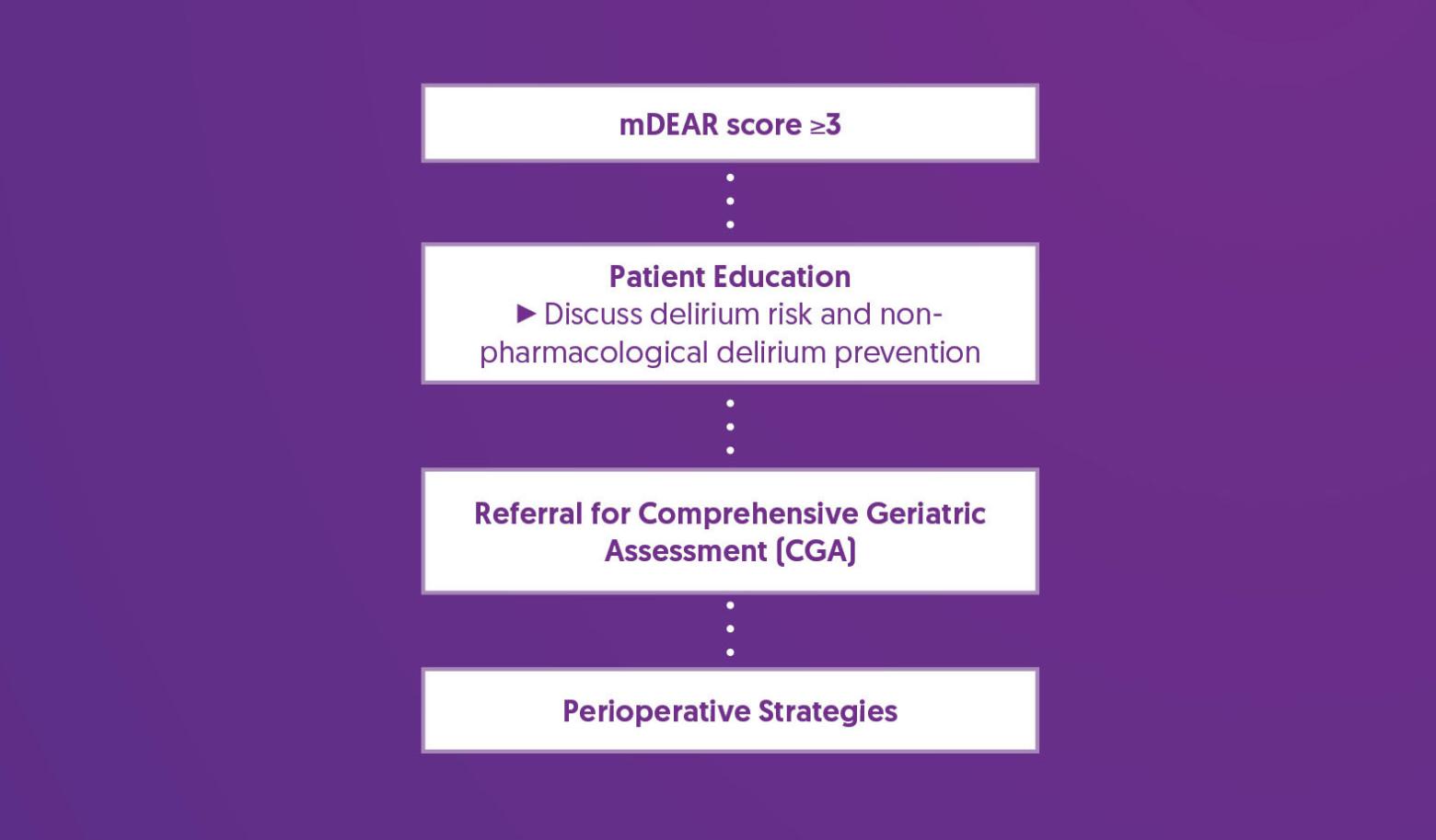
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Referral for Comprehensive Geriatric Assessment (CGA) |
|
| Perioperative Strategies |
|
References
1. Freter, S. H. (2005). Predicting post-operative delirium in elective orthopaedic patients: The Delirium Elderly At-Risk (DEAR) instrument. Age and Ageing, 34(2), 169–171. https://doi.org/10.1093/ageing/afh245
2. Freter, S., Dunbar, M., Koller, K., MacKnight, C., & Rockwood, K. (2015). Risk of Pre-and Post-Operative Delirium and the Delirium Elderly At Risk (DEAR) Tool in Hip Fracture Patients. Canadian geriatrics journal : CGJ, 18(4), 212–216. https://doi.org/10.5770/cgj.18.185
3. Zywiel, M. G., Hurley, R. T., Perruccio, A. V., Hancock-Howard, R. L., Coyte, P. C., & Rampersaud, Y. R. (2015). Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. The Journal of bone and joint surgery. American volume, 97(10), 829–836. https://doi.org/10.2106/JBJS.N.00724
4. Yan, E., Veitch, M., Saripella, A., Alhamdah, Y., Butris, N., Tang-Wai, D. F., Tartaglia, M. C., Nagappa, M., Englesakis, M., He, D., & Chung, F. (2023). Association between postoperative delirium and adverse outcomes in older surgical patients: A systematic review and meta-analysis. Journal of Clinical Anesthesia, 90, 111221. https://doi.org/10.1016/j.jclinane.2023.111221
5. Meehan, A. J., Gabra, J. N., Whyde, C. (2023). Development and validation of a delirium risk prediction model using a modified version of the Delirium Eldery at Risk (mDEAR) screen in hospitalized patients aged 65 and older: A medical record review. Geriatric Nursing, 51, 150-155.https://doi.org/10.1016/j.gerinurse.2023.03.003
6. Jin, Z., Hu, J., & Ma, D. (2020). Postoperative delirium: perioperative assessment, risk reduction, and management. British journal of anaesthesia, 125(4), 492–504. https://doi.org/10.1016/j.bja.2020.06.063