Approximately 10 per cent of patients in BC’s medical system believe they’re allergic to penicillin, but 90 per cent of those patients are wrong.
“It’s a big problem because people are getting antibiotics that aren’t optimal for their therapy, and it’s costing the health care system quite a bit of money,” says Dr Tiffany Wong, an allergist in the Division of Allergy and Immunology at BC Children’s Hospital.
Doctors must be pro-active, she explains. “While it may be easier to just avoid prescribing penicillin to patients claiming an allergy, it’s not necessarily the best for patient care.”
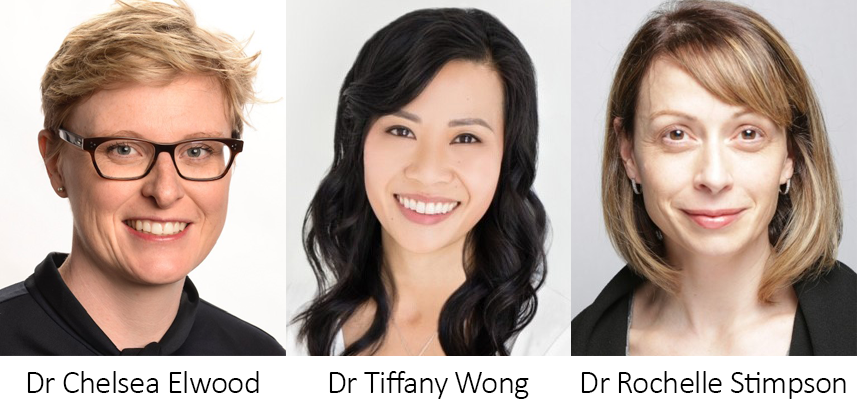
Dr Wong is one of three physicians working on projects to identify patients who are actually allergic to penicillin and to allay the fears of those who aren’t. Along with family physician Dr Rochelle Stimpson, of the BC Centre for Disease Control (BCCDC), and Dr Chelsea Elwood, a reproductive infectious disease specialist at BC Women’s Hospital, Dr Wong has developed and is trying to standardize a penicillin allergy de-labelling system. It includes a targeted assessment based on history-taking, possible skin testing and oral drug challenge to determine whether a patient is truly allergic to the antibiotic.
Many reactions attributed to penicillin allergy, such as diarrhea, are related to the side effects of medications, or are symptoms related to the illness being treated. Often the patient will tell their doctor about an allergy that was identified in childhood, without knowing how it was diagnosed. Having a true allergy means that allergy antibodies are directed at the allergen or the drug, and health professionals don’t always have the time or confidence to probe deeply into whether a claimed penicillin allergy really exists. The label “allergic to penicillin” then persists, preventing a patient from getting first-line medications.
Drs Wong, Stimpson and Elwood each have their own penicillin de-labelling programs, and their own target populations, at the institutions where they work. “What we’ve done is just come together to share resources,” says Dr Wong. As an allergist, she has specific expertise in drug allergy assessment and skin testing in challenges, and she provides leadership and guidance for the other projects.
Drs Wong and Stimpson discovered their mutual interest in penicillin allergy de-labelling while they were participating in the same cohort of Physician Quality Improvement (a flagship initiative of the Specialist Services Committee) in PHSA. Dr Stimpson works at the BCCDC’s Sexually Transmitted Infection (STI) clinic, where the patient-reported penicillin allergy was identified as an obstacle to optimal STI treatment.
Dr Wong learned about Dr Elwood, their third partner in this project, through the BC Women’s and Children’s Antimicrobial Stewardship Program, which Dr Elwood leads. She was establishing a multidisciplinary penicillin allergy de-labelling clinic for pregnant women at BC Women’s because 50 per cent of them receive an antibiotic during labour and delivery. If they are truly allergic to penicillin, the alternative treatments offered them may significantly affect care, while de-labelling them as allergic benefits them now and in any future pregnancies, Dr Elwood says. The clinic’s pilot program, run between July 2019 and March 2020, saw 66 pregnant women and de-labelled all of them.
At BC Children’s, Dr Wong’s multidisciplinary team sees both out-patients and in-patients participating in a research program. A pharmacist assesses each patient, tracing their history of reactions, and identifies those needing further testing. Dr Wong’s team also created an algorithm, now used by Dr Elwood, that rates whether each patient is low, medium or high risk for a penicillin allergy. Once that level of risk is determined, the team does the skin testing or oral challenge. It’s a one-time test with quick results.
Patients cleared of the allergy receive a document saying so. The team then updates all of the patient’s medical records, including those on PharmaNet, as best it can. Not all medical record-keeping is interwoven in BC.
Dr Wong has been working on penicillin de-labelling on an out-patient basis in the allergy clinic since 2015. Her objective since has been to help physicians who aren’t allergists to assess and de-label penicillin allergies. The out-patient Allergy Clinic at BC Children’s has already seen more than 200 patients, but the in-patient program has progressed slowly since its launch last December, partly due to Covid-19.
Dr Stimpson’s efforts at BCCDC were also affected by the pandemic and the resulting shift from in-person visits to virtual care. The physicians at the STI clinic continue to administer the penicillin allergy questionnaires to appropriate patients by phone or Zoom, but direct oral challenges are on hold for now.
Dr Wong is chair of a new Facility Engagement (another flagship initiative of the Specialist Services Committee) project establishing a BC penicillin allergy de-labelling network. Facility Engagement is another flagship initiative of the Specialist Service Committee. In addition, a mobile app called SPECTRUM, implemented for Antimicrobial Stewardship at BC Women’s and BC Children’s, will use her allergy questionnaire to identify penicillin allergies to stratify and manage risk in real time.
“We want this to be the standard of care in our institutions,” says Dr Wong, who hopes the de-labelling programs and mobile application will receive provincial funding. “We need our health authorities to put resources into sustaining this type of model, so it can continue.”



