Dr Carol Ward, a geriatric psychiatrist chose her specialty for the opportunity to connect with people. “I love stories. I love to hear people’s stories. And the longer you live, the better the story.” Growing up in the Maritimes, Dr Ward was surrounded by good story-tellers – “Generally speaking I find older folk are grateful and very appreciative of being able to share their lived experience.” Knowing her patients’ stories is her way to helping them. Dr Ward finds that it’s like being a detective – pulling all aspects of medicine and a person’s background together.
Dr Ward’s professional specialty was solidified while attending Queen’s University in Ontario where she was introduced to Dr Martin Rodenberg, one of the first geriatric psychiatrists in Canada. “In that moment I knew this was probably where I was going to go.”
Dr Ward’s career took her to Ottawa and later in 2005 to Kamloops where she, her husband, Dr Paul Dagg, and a dedicated team, helped to start Hillside Centre, a 47-bed acute tertiary mental health facility that serves older and younger adults in the Interior and the Northern Health authorities along with part of the provincial neuropsychiatry program. Working with colleagues, Dr Ward’s leadership has helped to introduce and develop a number of supports to enhance the care of these very complex patients.
In 2012, Dr Ward and tertiary mental health colleagues introduced P.I.E.C.E.S.™, which she learned about in Ontario. P.I.E.C.E.S.TM is a model that provides a shared understanding of the multiple underlying causes of behaviour in older individuals living with neurocognitive and other mental health disorders. It helps to inform the development of person-centred behavioural care plans with input directly from family members to bring together the patient’s story. Every caregiver that is involved with the patient then has the ‘care choreography’ to implement non-pharmacological support for behavioural symptoms.
Dr Ward cites an example of a 44-year-old patient with Alzheimer’s Disease who couldn’t stand still during care and would walk until she fell down. Through P.I.E.C.E.S.™ the care team found out from a family member that the patient loved pop music. As soon as the care providers played pop music, the patient started singing and was able to stay in one place for long enough to be provided with needed care. The care team also discovered that even though she was no longer talking, she could still sing.
In addition to patients, P.I.E.C.E.S.™ also benefits care providers who use this knowledge to be safer when dealing with behavioural issues that can escalate into aggressive behaviours. As a result of using this approach, patient’s aggression as well as the chances of them getting hurt are lowered, in addition to the potential extra advantage of curtailed psychotropic use.
For Dr Ward, knowledge transfer is key. Together with her colleagues, Dr Elisabeth Drance, Dr Barbara Prystawa and Mary Lou Harrigan, they developed and delivered an accredited workshop “Dementia-related Responsive Behaviour: Putting It All Together Using P.I.E.C.E.S.™ and the BC BPSD Algorithm” to primary care practitioners throughout the province. With funding from SSC, this training has now been developed into an online resource called ‘P.I.E.C.E.S.™ Dementia-related Behaviours’ located on the Interior Health’s YouTube channel. This video series consists of 11 short videos, on how to collaboratively build an effective care plan and approach to responsive behaviours that fits each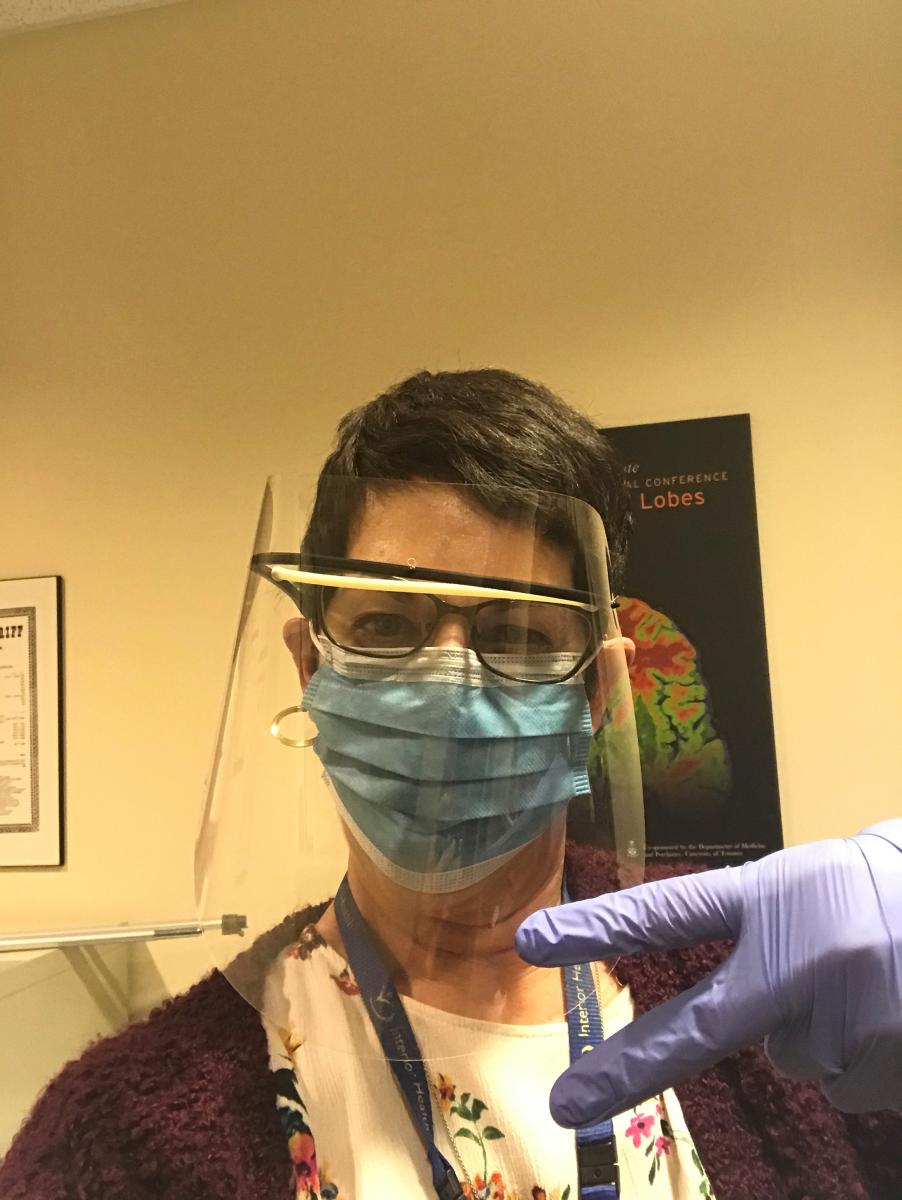 unique patient.
unique patient.
To support this work, IH long-term care leadership and Dr Ward received funding through SSC’s Quality and Innovation fund for her project titled “Enhancing Geriatric Services in Long Term Care.” This project started with enhancing and expanding a nurse liaison role known as a Regional Knowledge Coordinator (RKC) for Complex Behaviour for Long Term Care (LTC). RKCs support LTC sites with their expertise by building capacity for care through consultations, site visits, direct teaching and promotion of training supports, such as P.I.E.C.E.S.™, Gentle Persuasive Approach, the BC BPSD Algorithm (www.bcbpsd.ca), and more. Initially, the two-year pilot project funded 2.5 RKC positions but the success of the SSC project led to an IH commitment to continue funding for four RKCs-CB-LTC positions, making it a great example of the projects that start with SSC funding to fill a gap in care and that is sustained through health authorities and other health partners.
Since the majority of the geriatric psychiatrists working in BC are located in larger urban areas, it was also determined that rural physicians and nurse practitioners needed enhanced education and support in the management of older adults with complex mental health and substance use conditions. This led to Project ECHO (Extension for Community Health Care Outcomes) Mental Health and Substance Use within IH. Piloted with funds from the SSC project, the Ministry of Health Emergency Relief Fund and IH, Drs. Matt Burkey, Paul Carey and Dr Ward’s Project ECHO MHSU served to support a community of practice where primary care providers working in the 2017 wildfire affected areas of IH receive support and develop the skills they need to treat patients across the age continuum with complex MHSU issues. This is accomplished through case-based learning and best practices shared through the ECHO model using a virtual platform (ZOOM) and has continued with the support of the Canadian Red Cross.
Project ECHO has been a particularly effective tool to use during the COVID-19 crisis. In fact, this group developed a five-session pop up ECHO ‘Medical Staff Wellness in a Unique Time’ for physicians and nurse practitioners within IH to learn practical coping strategies for resiliency during COVID-19.
Dr Ward has found that her work has shifted since she first came to BC. While her clinical work continues, about 40 per cent of her time is leadership and QI work. She notes, “QI is not something I was trained to do in medical school, but I really enjoy the work.” She feels very fortunate to be supported in both clinical and leadership work through Interior Health and SSC and is proud of the friends and colleagues she’s made along the way. It is because of Dr Ward’s continuing work and commitment that elderly patients with complex issues and very diverse needs remain in good care.



