Before your surgery, it is important to take some time to think about what matters most to you and the kind of care you would want if a serious emergency happened while you are in the hospital. This includes the kind of care, treatments, and ways of living that you would or would not want.
Sometimes you may not be able to speak for yourself. Writing down your wishes helps your health care team and loved ones understand what is most important to you. This way, your care matches your values. Clear wishes can also guide your loved ones and give them comfort when making decisions on your behalf.
These conversations are not meant to scare you. They are meant to help in several ways:
- Make sure your care matches your values and wishes.
- Make sure that surgery is right for you.
- Reduce stress for you and your loved ones by thinking ahead.
- Let your health care team know your preferences if you cannot speak for yourself (for example, if you are under anesthetic or too ill to speak).
Who Needs to Talk About Goals of Care?
Your health care team might ask about what is important to you, what you want your life to look like after surgery, and what kinds of care you would or would not want. This may be called a "goals of care" conversation. These conversations are normal and routine before surgery.
They are especially common when:
- You do not have a written advance care plan or substitute decision maker
- You are having major surgery
- You are older, frail, or have multiple health conditions
If your health care team does not start this conversation with you, you can share your advance care plan or tell them what matters most to you.
What Can You Do Before Surgery?
Here are a few steps you can take now:
- Think about what matters most for your health and happiness
- Choose someone you trust to speak for you if you cannot. This is called a substitute decision-maker.
- Write down what is important to you and the types of treatment you would or would not want. The following tools can help with this:
- Share what you wrote with your substitute decision maker and/or your loved ones so they know your wishes.
Be Prepared for a MOST Conversation
Before surgery, your doctor (often your surgeon or anesthesiologist) will complete a Medical Orders for Scope of Treatment (MOST). This order tells the health care team what treatments you want if your health gets worse during or after surgery.
Some treatments included in a MOST order are::
- CPR (chest compressions or electric shocks to your heart)
- Being on a breathing machine beyond surgery
Your MOST order can be updated at anytime if your health or wishes change. It will always reflect the most recent conversation.
The graphic and video linked below can help you make decisions about Cardiopulmonary Resuscitation (CPR).
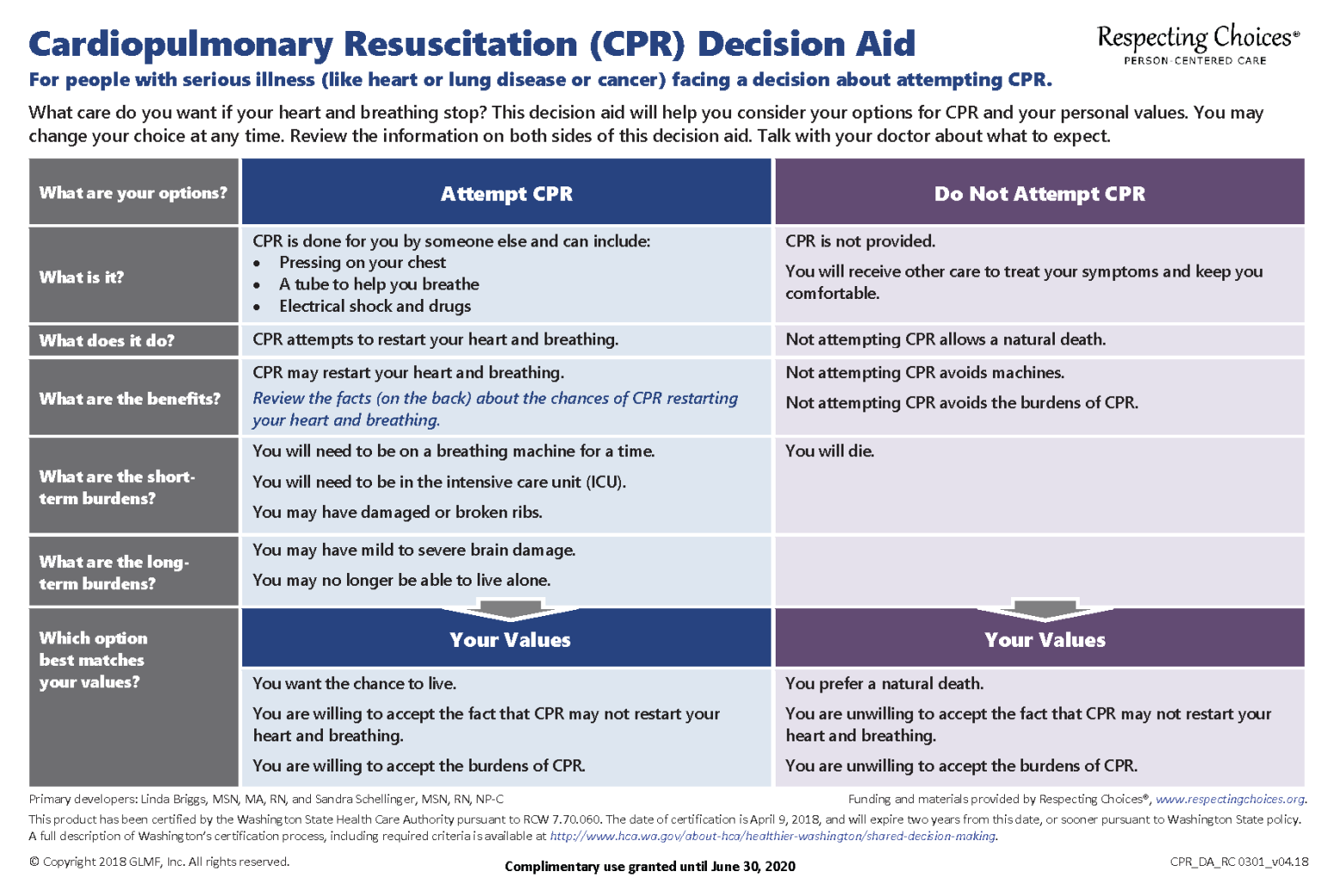
Watch this Video on Preparing Patients and Their Families for Shared Decision-Making About Cardio-Pulmonary Resuscitation