Purpose
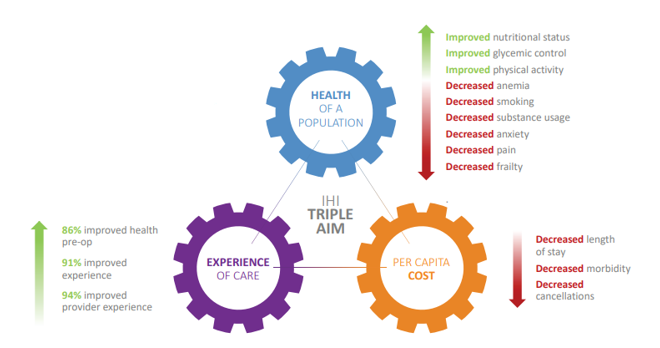
Surgical patient optimization is a multidisciplinary, structured, and personalized prehabilitation program designed to assist patients in preparing for surgery. Prehabilitation before major surgery can lead to a faster recovery, better patient experiences and outcomes, and savings for the health care system. Best practices for surgical prehabilitation focus on both mental and physical aspects of surgery by decreasing presurgical risk factors and increasing a patient’s functional capacity. Surgical Patient Optimization Collaborative (SPOC) improves the experience for surgical patients by:
- Using a patient-centered and multidisciplinary approach.
- Supporting care providers to implement change processes.
- Using preoperative surgical wait times.
- Integrating available community resources.
- Improving patient outcomes.
Sizing it Up
SPOC has implemented interactive, multi-disciplinary learning fueled by in-person learning sessions and action periods, designed to support the implementation of prehabilitation processes and components. Teams are supported throughout the period of the collaborative to create a sustainable prehabilitation process in order to be able to continue this work beyond the time period of the collaborative.
Things to Know
BC Surgical Patient Prehabilitation is designed to assist patients to prepare for an elective procedure, so they experience improved outcomes from their surgery. It focuses on both the mental and physical aspects of surgery, therefore decreasing pre-surgical risk factors so that patients can obtain high quality outcomes from their surgery. Components of prehabilitation include:

Access Support
Applications for the second cohort (2022/23) are now closed.
-
Resources
-
SPOC Initiative Information Sheet
BC Surgical Prehabilitation Toolkit
Surgical Patient Prehabilitation Implementation Toolkit
Spread and Sustainability Resource Cards
Patient Passport for Surgical Prehabilitation
-
Videos
-
BC Surgical Patient Prehabilitation - Overview
BC Surgical Patient Prehabilitation - Frailty
BC Surgical Patient Prehabilitation - Anemia
BC Surgical Patient Prehabilitation - Cardiac
BC Surgical Patient Prehabilitation - Weight Loss
BC Surgical Patient Prehabilitation - Anxiety
BC Surgical Patient Prehabilitation - Smoking Cessation
BC Surgical Patient Prehabilitation - Sleep Apnea
BC Surgical Patient Prehabilitation - Substance Use
BC Surgical Patient Prehabilitation - Physical Activity
BC Surgical Patient Prehabilitation - Nutrition
BC Surgical Patient Prehabilitation - Pain
-
SPOC Outcomes Congress
-
2023
- Watch the recording of the webinar from September 23, 2021.
00:00:00 | Welcome
00:05:54 | Dr Ahmer Karimuddin, Prehabilitation and the BC Landscape
00:18:00 | Overview of the Collaborative
00:56:00 | The SPOC Patient Experience
01:08:47 | The SPOC Site Experience- Burnaby Hospital
01:23:28 | Evaluation Findings
01:35:10 | Economic Evaluation Findings
01:52:49 | Next Steps and Thank You
-
-
Webinars
-
Surgical Patient Optimization Collaborative (SPOC) All Team Webinar #8
Surgical Patient Optimization Collaborative (SPOC) All Team Webinar #7
Surgical Patient Optimization Collaborative (SPOC) All Team Webinar #6
Surgical Patient Optimization Collaborative (SPOC) All Team Webinar #5
Surgical Patient Optimization Collaborative (SPOC) All Team Webinar #2
Contact
Geoff Schierbeck, Portfolio Liaison: gschierbeck@doctorsofbc.ca.
An initiative of the Specialist Services Committee, SPOC is also supported by the Shared Care Committee and Family Practice Services Committee—three Joint Collaborative Committees that represent a partnership between Doctors of BC and the BC Government.
- Community Based Specialists
- Consultant Specialist Team Care
- Facility Engagement
- Health System Redesign
- Physician Quality Improvement Initiative
- Physician Leadership Development
- UBC Sauder Physician Leadership Program
- Specialists Well-Being Pilot (SWELL)
- Perioperative Clinical Action Network (PCAN)
- SSC Fees



