Getting Ready for Surgery: A Patient's Guide to Prehabilitation
Supporting patients in British Columbia on their surgical journeys
WHAT IS PREHABILITATION?
Research has shown that improving certain health factors before surgery can have a positive effect on surgical outcomes. You can use the wait time before your surgery to improve components of your health in order to have better outcomes. This includes things like improving your physical activity, mental wellbeing, and nutrition, and optimizing medical conditions like anemia, diabetes, and sleep apnea. The following pages provide information about different components of your health and things you can do to improve them before surgery.
Download a PDF version of the patient guide by clicking the image below, or access each health factor through the icons below or the menu on the left.
Legal Disclaimer
We try very hard to keep this information accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this information as a guide. This information on its own should not be treated as advice. It cannot be used for any commercial or business purpose. Although we make reasonable efforts to ensure the accuracy of the information in these resources, we make no representations, warranties or guarantees, whether express or implied, that the information is accurate, complete, or up to date. We do not exclude or limit in any way our liability where it would be unlawful to do so.
© 2025 Specialists Services Committee
This information may be copied for the purpose of producing information materials. Please quote this original source. If you wish to use part of this information in another publication, suitable acknowledgement must be given and the logos, branding, images, and icons removed. For more information, please contact us at sscbc@doctorsofbc.ca.
SSC. (2025). Getting Ready for Surgery: A Patient’s Guide to Prehabilitation. www.sscbc.ca/patient-prehab-guide
Alcohol & Surgery: What You Need to Know
Avoiding alcohol before surgery is important to help your body heal faster and reduce risks. Even small amounts of alcohol can affect how your body responds to surgery and medications. Stopping or cutting back before surgery helps your body heal faster and reduces risks.
If you drink alcohol every day, your body may be dependent. Stopping suddenly can cause dangerous withdrawal symptoms. Always talk to your doctor or health care team before making changes.
Benefits of avoiding alcohol include:
- Faster healing and shorter hospital stays
- Stronger lungs
- Reduce risk from anesthesia and medications
- Lower your chance of complications
Why We Ask About Alcohol Use Before Surgery?
If you drink alcohol, even occasionally, it is important to understand how it can affect your surgery and recovery. This information is shared with all patients who drink any amount of alcohol, so everyone take steps to stay safe and heal well.
What Can You Do Before Surgery?
You should not drink any alcohol for at least 24 hours before your surgery. However, if you drink alcohol every day or almost every day, stopping suddenly may cause dangerous withdrawal symptoms and you may need a plan to safely reduce or taper alcohol use with medical support. Always talk to your health care team before making changes.
Follow Canada's Low Risk Drinking Guidelines:
- 0 drinks per week = best health benefits (including better sleep, heart, and brain health)
- 1-2 drinks per week = low risk of alcohol-related harms
- More than 7 drinks per week (women) or 14 drinks per week (men) = increased health risks
No type of alcohol is safer than another - wine, beer, spirits, cider, all carry the same risks.
Symptoms of alcohol withdrawal may include:
- Feeling shaky or anxious
- Nausea (feeling sick to your stomach) or sweating
- Confusion or hallucinations (seeing things that are not there)
- Seizures
If you have ever had these symptoms after stopping alcohol, it is important to tell your health care team. We are not here to judge, we are here to keep you safe. You may need medication in the hospital to stay safe.
How to Get Help Before Surgery
If you are ready to reduce or quit alcohol:
- Talk to your family doctor or nurse practitioner about a safe plan - there are medications available that can help with quitting
- Call *811 to speak with a health navigator for local resources
- Call the 24-hour Alcohol and Drug Information Line at 1-800-663-1441
There is no shame in asking for help. We bring this up because alcohol can seriously affect your surgery, and we want you to have the safest recovery possible.
Where to Learn More
Learn more about substance use at Healthlink BC or call *811
Visit Help Starts Here for substance use and addictions support.
Call BC *211 or visit bc.211.ca to find community and social resources close to home.
24-hour BC Alcohol and Drug Information and Referral Service: 1-800-663-1441
Canada's Low Risk Alcohol Guidelines
First Nations Health Authority Mental Health and Substance Use
Anemia & Surgery: What You Need to Know
Anemia is the medical word for low red blood. Red blood cells carry oxygen, which gives your body energy and helps your brain work well. When someone has anemia, they may feel tired, weak, short of breath, or find it harder to focus.
Anemia can be caused by:
- Low iron stores in the body
- Blood loss
- Certain health conditions
Getting anemia treated before surgery can:
- Lower your chance of needing a blood transfusion
- Make recovery easier and faster
- Lower your risk of complications
Treating your anemia before surgery can make your surgery safer and help you recover faster.
How is Anemia Found?
Before surgery, your doctor will ask you questions about your health and may order a simple blood test. This test checks your hemoglobin level (the part of the red blood cell that carries oxygen).
If your hemoglobin is low, your health care team may do more tests to find out why. For example, they may check your iron levels, kidney health, or look for other medical conditions.
What Can You Do Before Surgery?
If you learn you have anemia, it is a great idea to book an appointment with your primary care provider to figure out the cause. Some hospitals also have special programs to help patients with anemia get ready for surgery. Depending on your health and type of surgery, you may need more tests or to see a specialist.
If low iron is the reason for your anemia, you may be asked to build up your iron levels by:
- Eating more foods with iron like meat, fish, poultry, beans, peas, or lentils (check out the Nutrition section for more examples)
- Taking iron pills at home
- Getting iron through an IV infusion at the hospital
Your health care team may check your blood again before surgery to see how well the treatment is working.
Where to Learn More
Healthlink BC - Learn more about Anemia and how to manage it
Blood Sugar (Glucose) Control & Surgery: What You Need to Know
Keeping your blood sugar (glucose) in a healthy range is very important when you are getting ready for surgery. This means not too high and not too low. It matters most if you have diabetes or trouble with blood sugar control.
Getting your blood sugar into a healthy range before surgery helps your stay safer and heal faster.
Healthy blood sugar levels:
- Help your wounds heal faster
- Decrease your chance of infections
- Support a faster recovery
- Keep your immune system strong
How Do We Check Blood Sugar?
Your health care team may order a blood test to check your blood sugar if you are in one of two groups:
- You are being screened for diabetes or pre-diabetes
- You already have diabetes or pre-diabetes
You may be screened for diabetes or pre-diabetes if:
- You are over the age of 40
- You have a family history of diabetes
- You have had high blood sugar in the past
- You have other risk factors
By checking your blood sugar early, your health care team can make the best decisions to keep you safe and support a smooth recovery.
What Can You Do Before Surgery?
If you have diabetes, pre-diabetes, or higher blood sugar, there are steps you can take to help your body get ready for surgery.
What is the goal?
- Target: A hemoglobin A1c (HbA1c) below 7 is best for safe recovery.
- Flexibility: For some people, this target may not be realistic - and that is okay. Your health care team will help you find a safe and reasonable plan.
- Risk: If your HbA1c is above 8.5, some surgeries may need to wait until your blood sugar is better controlled.
To help you reach your goal, your health care team may refer you to your primary care provider or a diabetes educator to help you with medication changes, nutrition, and lifestyle planning.
Even a few weeks of better blood sugar control can make a difference. Try to:
- Take your medications as prescribed and follow your diabetes treatment plan
- Eat balanced meals with fewer sugary foods and more vegetables, fibre, and protein (refer to the Nutrition section for more information)
- Stay active - walking can help blood sugar control (refer to the Getting Active Before Surgery section for more information)
- Avoid smoking and alcohol, which can slow healing and blood affect blood sugar
- Track your blood sugars (if you can) and share your readings with your health care provider
If you need help or are not sure what steps to take, talk to your health care team.
Where to Learn More
Healthlink BC - Diabetes
First Nations Health Authority - Health Living with Diabetes
Cannabis (Marijuana) Use & Surgery: What You Need to Know
Using cannabis (marijuana) can affect your body during and after surgery. Cutting back or stopping cannabis use before surgery can:
- Make your breathing and lung health better
- Lower stress on your heart
- Reduce the amount of pain medication you need
- Decrease nausea and vomiting
- Prevent reactions to anesthesia (the medicine that puts you to sleep during surgery)
Why We Ask About Cannabis Use Before Surgery?
Cannabis can change how your body reacts to anesthesia and pain medicine. We share this information with everyone who uses cannabis so you can prepare safely and have the best possible recovery.
What Can You Do Before Surgery?
If you use cannabis under the supervision of a medical provider, speak with them about whether you should decrease or stop your use before surgery.
If you use cannabis occasionally (less than 4 days per week)
- Stop using it at least 72 hours (3 days) before surgery.
- This includes smoking, vaping, edibles, and oils - but not topical creams.
- If you are intoxicated (high) on the day of surgery, your surgery will be delayed or cancelled unless it is an emergency.
Being high can seriously affect how your body responds to surgery and may even put your life at risk.
If you use cannabis daily or in large amounts
You are considered a heavy user if you:
- Smoke or vape more than 1.5 grams per day
- Use more than 300 mg per day of CBD (oil, edibles, etc.)
- Use more than 20 mg per day of THC (oil, edibles, etc.)
- Use cannabis 2 or more times per day, or use unknown or high-dose products regularly
If this applies to you:
- Stopping suddenly can cause unpleasant withdrawal symptoms (cannabis withdrawal syndrome).
- Try to slowly reduce the amount you use each day over 7 days, then stop at least 72 hours before surgery.
Cannabis Withdrawal Syndrome (CWS)
Withdrawal from cannabis is not dangerous, but quitting suddenly can make you uncomfortable.
Symptoms may include:
- Trouble sleeping
- Anxiety or irritability
- Headaches or stomach upset
These usually begin 1-2 days after stopping and may last up to 3 weeks. Cutting back slowly can reduce or prevent these symptoms.
Follow Canada's Lower Risk Cannabis Use Guidelines
- Use less often - fewer days per week means fewer health risks
- Choose products with more CBD and less THC - high THC levels increase the chance of side effects like anxiety and memory problems
- Avoid smoking cannabis to protect your lungs from damage and decrease your risk of complications after surgery
- Avoid mixing cannabis with alcohol or other substances to reduce your risk of accidents and health problems
- Avoid synthetic cannabis products - these can be unpredictable and dangerous
- Buy from a licensed cannabis store - that way, you know exactly what is in your product (THC/CBD levels, additives) and avoid harmful contaminants
How to Get Help Before Surgery
If you are ready to reduce or quit cannabis:
- Talk to your family doctor or nurse practitioner
- Call *811 to speak to a health navigator
- Ask your health care team to refer you to an Addiction Medicine specialist
- Some people may also meet with an anesthesiologist before surgery to plan pain management and anesthesia safely
Where to Learn More
Learn more about Cannabis Use at HealthLink BC
Visit Help Starts Here for resources and support for Substance Use
Visit bc.2111.ca or call *211 for community resources
Canada's Lower Risk Cannabis Guidelines
First Nations Health Authority Non-Medical Cannabis Information
Delirium (Sudden Confusion) & Surgery: What You Need to Know
Delirium is type of sudden confusion that can happen after surgery. Delirium is more common in older adults and people with certain health conditions. It affects about 1 in 5 people after a big surgery. If it happens, it is important to know that it is often temporary and treatable.
Someone with delirium may:
- Feel mixed up of confused, including forgetting that they are in a hospital and are safe
- Have trouble paying attention
- See or hear things that are not really there
Delirium can start quickly and may feel upsetting for patients and their loved ones.
How Do We Check For Delirium Risk?
Some people have a higher chance of getting delirium after surgery. This can depend on things like your age, memory, the medicines you take, your overall health, and how big your surgery is.
Your health care team may ask you questions about your health and daily activities to see if you may be more likely to get delirium and if you may need extra support during and after surgery.
Even if you have a higher chance of experiencing delirium, it does not mean it will happen. Instead, it gives your health care team a chance to:
- Take steps to lower your risk
- Help you and your loved ones get ready for surgery
- Share tips on how to spot the signs of delirium and get help if needed
What Can You Do?
There are many things you can do before and after surgery to help lower your risk of delirium and support your healing.
Before Surgery: Set Yourself Up for Success
Here are helpful things you can do take:
- Stay active - Even short daily walks can keep your body and mind strong before surgery (Refer to the Getting Active Before Surgery section for more information).
- Eat well - Choose balanced meals with enough calories and protein to give your body energy for healing (Refer to the Nutrition section for more information).
- Cut back on alcohol, cannabis, and smoking - Cutting back or stopping can help your brain stay sharp. If you drink alcohol every day, your body may be dependent and stopping suddenly may cause withdrawal symptoms. Talk to your health care team before making changes (Refer to the Alcohol, Cannabis, and Smoking sections for more information).
- See a geriatrician (if recommended) - These doctors specialize in the care of older adults and can help review your health and medicines to help protect your memory and thinking.
After Surgery: Helping Your Brain Stay Clear
There are many simple things that make recovery easier:
- Wear your glasses and hearing aids - Seeing and hearing well helps you stay connected and makes it easier to talk with your health care team.
- Keep a day-night routine - Stay awake during the day (open the curtains, keep lights on) and sleep at night (close blinds, turn off lights). This helps your body's natural clock stay on track.
- Bring familiar items - A clock, calendar, or family photo can help you know where you are and feel more comfortable.
- Have family or friends nearby - A calm, familiar voice can comfort you and remind you where you are if you feel confused.
- Manage pain and discomfort - Your health care team will help you with pain control.
- Drink plenty of fluids - Staying hydrated helps your body heal and lowers your chance of confusion.
- Start moving - Sitting up in a chair or taking short walks can help your brain recover from surgery.
- Keep your mind active - Books, games, or other activities can help your brain stay engaged as you recover.
Delirium can be upsetting, but it is temporary and there are many ways to prevent or manage it. Your health care team and loved ones are here to support you. By following these steps, you are giving yourself the best change of healing safely and fully.
Where to Learn More
Delirium Prevention and Care with Older Adults pamphlet
Video about Postoperative Delirium (for Patients and Caregivers)
Frailty & Surgery: What You Need to Know
Frailty is when someone's body has become weaker and may be less able to bounce back from stress like illness, injury, or surgery. It often means someone may have less strength, energy, or muscle, and everyday tasks might feel harder.
People living with frailty may:
- Walk more slowly
- Feel tired more often
- Lose weight without trying
- Find it harder to think clearly or remember things.
Frailty usually develops slowly over time and often happens when someone lives with long-term health problems. The good news is that there are ways to support your health and build strength, especially before surgery.
Even if someone living with frailty looks or feels fine day-to-day, becoming stronger before surgery can help to:
- Decrease complications during or after surgery
- Decrease falls or weakness after surgery
- Shorten time in hospital and make recovery faster
- Stay independent or return to usual activities more quickly
- Decrease the need for home support or moving to a more supported living environment
How Do We Know if Someone is Living With Frailty?
Your health care team may use something called the FRAIL Scale. It is a short set of questions that helps identify if someone is living with frailty. It is not perfect, but it is a good starting point. If the answers suggest you many be living with frailty, your health care team can take a closer look and give you support to help improve your health and recovery from surgery.
The FRAIL Scale questions are:
- Have you felt tired or had low energy most or all of the time in the past month?
- Is it hard to climb one flight of stairs without resting?
- Is it hard to walk one block (about 100 meters)?
- Do you have five or more long-term health conditions (like high blood pressure, high cholesterol, or diabetes)?
- Have you lost more than 5% of your body weight in the past 6 months without trying?
What Can You Do Before Surgery?
Sometimes your health care team may suggest you see a geriatrician, who is a doctor that specializes in caring for older adults and people with complex health needs. They can:
- Review your medications, medical history, diet, and overall health
- Check your memory and thinking
- Help you stay as strong and healthy as possible before surgery
- Share ways to protect your brain before and after surgery
Remember: you are not alone. Your health care team is here to support you every step of the way. The goal is to make your surgery and recovery as safe, smooth, and personal as possible.
Get Moving the Right Way for You
Improving your physical strength and balance before surgery can help you:
- Heal faster
- Stay steady and avoid falls
- Get your independence back sooner
Healthlink BC's Strength and Balancing Exercise (STABL) programs
Free home exercise programs that are available as a follow along video or a PDF handout.
- 3 levels - sit, stand, and move.
- Choose the level that feels right for you and repeat it 2 days per week.
STABL - Level 2 - Stand Handout
STABL - Level 3 - Move Handout
People with frailty often need extra support to get moving safely. Here are some options for additional support.
Choose to Move |
A free 3-month program to help you be more active in a way that works for you.As part of the program, you will:
Go to choosetomove.ca/register to join. You will receive a registration package via email with the online and in-person options. |
Clinical Exercise Physiologist |
Clinical Exercise Physiologists are available for free through HealthlinkBC. They can help you with:
Call *811 (*711 for hearing impaired) or connect by email |
Physiotherapist |
Physiotherapists can help you make a personal plan to safely build strength and stamina before surgery. To connect with a Physiotherapist:
|
Fuel Your Body With the Right Nutrition
Eating well gives your body the power to heal. Many people living with frailty do not eat enough calories or protein, which can slow recovery. Check out the Nutrition section for more information about health eating habits before surgery.
A dietitian can help you understand what your current diet may be missing and give you ideas to meet the guidance above. To contact a dietitian::
- You do not need a referral to see a dietitian
- Contact a dietitian through HealthlinkBC by calling *811 or by email
- Visit BCdieticians.ca to find a dietitian near you.
- Dietitian services are not covered by MSP, but are covered by many extended health benefits and insurance plans.
Where to Learn More
Healthlink BC - Aging well
Parachute Canada - Fall Prevention
HealthLink Strength and Balance for Life (STABL) Level 1 - Sit
HealthLink Strength and Balance for Life (STABL) Level 2 - Stand
HealthLink Strength and Balance for Life (STABL) Level 3 - Move
HealthLink Strength and Balance for Life (STABL) Videos
Choose to Move - Activity Coaching
HealthlinkBC - Connect with a Certified Exercise Physiologist
HealthlinkBC - Connect with a Dietitian
BCPhysio.org - Find a Physiotherapist
BCDietitians.ca - Find a Dietitian
Getting Active Before Surgery: What You Need to Know
Being active before surgery helps your heart, lungs, and muscles work better. This makes is easier for your body to heal faster and with fewer problems. If your body is stronger before surgery, you are more likely to:
- Avoid infections
- Breathe easier after anesthesia
- Spend less time in the hospital
- Be independent at home
Even just a few weeks of regular activity can make a big difference!
What Are The Guidelines For Physical Activity?
The Canadian Physical Activity Guidelines and the World Health Organization suggest for adults:
- At least 150 minutes (2.5 hours) of moderate activity per week (like brisk walking or cycling)
- Plus 2 days per week of strength and balance activities
If you are not doing this yet, do not worry! Keep reading for tips and resources to get started.
What Can You Do Before Surgery?
Being on a wait list for surgery is the perfect time to get prepared! You do not have to join a gym or run a marathon - just move more, starting now. Below are some suggestions to get started.
Improving your strength and balance before surgery is especially helpful for your recovery after surgery. If your medical condition(s) or pain limits your ability to exercise, read on for additional support.
Strength and Balance Activities - 2 days per week
HealthlinkBC's Strength and Balancing Exercise (STABL) programs are a good place to start and are available as follow along videos or PDF handouts below. There are 3 levels - Sit, Stand, and Move. Choose the level that feels right for you and complete it 2 days per week.
STABL - Level 2 - Stand Handout
STABL - Level 3 - Move Handout
Aerobic or Fitness Activies - Aim for 30 minutes per day, 5 days per week
A brisk walk (where you can talk, but not sing) is the easiest way to get started or consider other activities like biking, gardening, dancing, swimming or pool walking, or using an elliptical machine or exercise bike.
Deep Breathing Exercises - Daily
It is important to do deep breathing exercises immediately after surgery and every hour while in hospital while you are awake. Practicing this ahead of surgery makes it easier to remember and strengthens your lungs for during and after surgery. This lowers your risk of pneumonia and speeds up recovery.
- Place your hand on the front of your stomach. Expand your stomach into your hand as you breathe in deeply for 3 seconds.
- Hold for 3 seconds.
- Breathe out slowly through pursed lips for 3 seconds. Do not force your breath out.
- Repeat 10 times. Rest if you become dizzy or lightheaded.
Options for Additional Support
Choose to Move |
A free 3-month program to help you be more active in a way that works for you.As part of the program, you will:
Go to choosetomove.ca/register to join. You will receive a registration package via email with the online and in-person options. |
Clinical Exercise Physiologist |
Clinical Exercise Physiologists are available for free through HealthlinkBC. They can help you with:
Call *811 (*711 for hearing impaired) or connect by email |
Physiotherapist |
Physiotherapists can help you make a personal plan to safely build strength and stamina before surgery. To connect with a Physiotherapist:
|
Where to Learn More
HealthLink Strength and Balance for Life (STABL) Level 1 - Sit
HealthLink Strength and Balance for Life (STABL) Level 2 - Stand
HealthLink Strength and Balance for Life (STABL) Level 3 - Move
HealthLink Strength and Balance for Life (STABLE) Videos
Choose to Move - Activity Coaching
HealthlinkBC - Connect with a Certified Exercise Physiologist
BCPhysio.org - Find a Physiotherapist
Heart Health & Surgery: What You Need to Know
Having surgery is a big event which causes stress on your body systems including your heart. While many patients have surgery without complications, some patients are at higher risk of serious heart problems around the time of surgery, including:
- A heart attack (when the heart muscle does not get enough blood)
- An irregular heartbeat (arrhythmias)
- Heart failure (when the heart muscle is weak and cannot pump blood well)
- Cardiac arrest (when the heart stops beating and it may, or may not, be possible to start it again)
Because your heart can work extra hard during and after surgery, your health care team may check your heart carefully before surgery to learn how well your heart is working and help estimate your potential heart risk.
Knowing your risks helps your health care team plan ahead and take steps to monitor, support, and protect your heart before, during, and after surgery. It also gives you helpful information about your health so you can make decisions about surgery.
How Does Your Health Care Team Check Your Heart?
Your health care team may:
- Ask about your medical history and symptoms you are having
- Do a physical exam
- Do blood tests or an electrocardiogram
This information is used to help predict your personal risk of serious heart problems after surgery. Your health care team can explain what the results mean and answer any questions you have. They may also order additional tests or refer you to a specialist.
What Can You Do Before Surgery?
There are many things you can do to help protect your heart before surgery. These can make recovery smoother and safer.
- Optimize your heart issues and conditions that affect the heart - Work with your health care team to make sure your blood pressure, heart rate, and other conditions are be well managed.
- Share symptoms with your doctor, especially if new or worsening - Before surgery, tell your health care team If you have had chest pain, shortness of breath, dizziness, or fainting. These symptoms may need attention and sharing them helps your health care team treat any issues early and avoid delays in surgery.
- Be open to extra testing or a specialist visit - If your health care team suggests more heart tests, these can give important information to guide your care and make sure surgery is safe for you.
- Develop healthy habits while waiting for surgery - This will ensure your heart is as strong as possible before surgery. Check out the Getting Active, Nutrition, and Smoking Cessation sections.
Where to Learn More
Healthlink BC - Information on heart health
Cardiac Services BC - Information on heart failure and heart rhythm disorders
Managing Pain After Surgery: What You Need to Know
It is normal to feel some discomfort after surgery. This is your body's way of saying, "This area is healing, take care."
Trying to take away all discomfort with strong medicines is not possible without causing serious side effects. These medicines (like opioids) can help, but if used too much they can also cause nausea, constipation, trouble breathing, or confusion.
This is why your health care team focuses on function - using different types of medications and other strategies to make sure you can do the things you need to do to recover, such as:
- Breathe deeply
- Do your exersices or physiotherapy
- Get up and move
- Rest and sleep
These activities are the most important part of recovery and are the goal of pain management.
How Do We Know Who Needs More Support?
Some people are at higher risk of having pain or discomfort that is harder to manage after surgery. This can happen if you already live with chronic pain, if you take opioid medicines regularly, or if you have had challenges with pain control in the past. Your health care team may give you extra information and ask you questions so they can make a plan that is right for you.
What Can You Do Before Surgery?
Tell your health care team about your health history, medicines you take, and any worries you have about managing discomfort. Together, you will make a safe plan.
Access Free Online Resources
- Managing Pain Before and After Surgery - free online self-directed course from Pain Canada
- Empowered Relief - free online class teaching ways to manage discomfort
- Power Over Pain Portal - collection of tools and education
- Coaching for Health - free one-on-one telephone coaching for people living with chronic pain
- Gentle Movement at Home - free video series on YouTube by Pain BC
Access Specialized Pain Care
The options below require a referral from your health care provider.
- Mind-Space - online group programs for mental health, sleep, and coping with pain
- Chronic Pain Clinics - for people with daily discomfort lasting more than 3 months
- Transitional Pain Clinics - short-term programs to help with comfort before and after surgery (available for surgeries in Vancouver Coastal Health and Providence Health)
Meet With Your Anesthesiologist
An anesthesiologist is a doctor that helps with comfort and safety during and after surgery. Before surgery, you might meet with one to:
- Plan how to manage discomfort during and after surgery
- Learn about options besides opioid medicines
- Understand what to expect in recovery
If you need more support to stay functional and comfortable while healing from surgery, your health care team is here to help. Together you can plan ahead and find the right tools.
Where to Learn More
Visit Pain BC or Pain Canada to access free resources for pain management.
Mental Wellbeing & Surgery: What You Need to Know
Your mind and body work together. Your thoughts can change how your body feels and your body can change how your mind feels. For example, when we feel scared, our heart may beat faster, and when we experience physical pain, we can feel sad. This is called the mind-body connection.
It is normal to feel nervous before surgery, but if strong feelings of worry or sadness last for many days, they can make healing slower.
Good mental health before and after surgery can:
- Help you feel better
- Lower your pain
- Help you heal faster
- Lower the chance of complications
How Do We Check For Anxiety and Depression?
You may have answered some questions about how often you feel worried or sad. These questions help your heath care team understand how you have been feeling so they can offer extra support to help you prepare for surgery and recover from surgery more smoothly.
What Can You Do Before Surgery?
It is important for you to feel that your mental health is being supported before and after surgery. Simply talking about how you are feeling with someone supportive can reduce your worries. This can be your family doctor, a counsellor, or even a friend or family member. Below are some online and phone resources if you do not have someone you can talk to.
- Help Starts Here - online information about mental wellbeing and accessing supports in BC
- Anxiety Canada - online resources to help manage anxiety and worry
- BounceBack - free, skill-building program available online or over the phone to manage low mood, mild to moderate depression, anxiety, stress, or worry
- *211 or bc.211.ca - access local supports and resources for mental health
- First Nations Health Authority - Indigenous specific resources for wellness
- Ask your health care team in a referral to Mind-Space.ca is right for you. Mind Space offers virtual group medical visits to help patients with mild to moderate anxiety (feeling worried or nervous), depression (feeling sad or low mood), stress, insomnia (trouble sleeping), and ADHD.
If You Are In Crisis and Need Immediate Help
- National Suicide Crisis Helpline: Call or text *988
- BC Mental Health and Crisis Response Line: 310-6789 or 1-800-SUICIDE
- Kids Help Phone: Text CONNECT to 686868 or call 1-800-668-6868
- KU-UUS First Nations and Aboriginal Crisis Support Line: 1-800-588-8717
Tips and Tools to Help You Feel More Calm Before Surgery
Sometimes life feels busy and stressful. Paying attention to your own thoughts, feelings, and what is happening around you right now can help your mind and body feel better. This is called being mindful. Mindfulness means focusing on the present moment instead of worrying about the past or the future.
It can help to learn a few quick tools to calm yourself down when you feel stressed. Pick one or two that you like best and practice them even on days when you do not feel stressed. That way, they will be easier to use when things feel harder.
| Mindful Breathing |
|
| The Physiologic Sigh |
|
| Progressive Muscle Relaxation |
|
| 5-4-3-2-1 Exercise |
|
| Self-Compassion |
|
A Healing Mindset After Surgery
A healing mindset means using your thoughts to help your body get better. It includes noticing your feelings, thinking in positive ways, and believing you can heal.
How to Cultivate a Healing Mindset:
- Practice Awareness: Pay attention to your body and thoughts. For Example: "I feel tightness where my stitches are".
- Shift Your Story: Instead of thinking "Why am I in pain?" try thinking "This is my body's way of telling me this area needs care." Discomfort can be a reminder to rest, move gently, or use breathing exercises.
- Use Visualization: Close your eyes and picture your body healing. Imagine your breath carrying calm and strength to the part of you that feels sore.
- Engage Stillness: Try short moments of quiet - breathe slowly, listen to music, or sit in nature.
- Surround Yourself Wisely: Healing mindsets are contagious. Spend time with people who encourage you and believe in your recovery.
Where to Learn More
HealthlinkBC - Mental health information and resources
Help Starts Here - Information about mental wellbeing and access to support in BC
Anxiety Canada - Information about managing anxiety
BounceBack - Online programs for mental wellbeing
Royal College of Anesthestists - Preparing Your Mind Before Surgery
First Nations Health Authority - Indigenous specific resources for wellness
Nutrition & Surgery: What You Need to Know
One of the best things you can do before surgery is to focus on eating well. This is really important if you have lost weight without trying or have noticed changes in your appetite in the past week or more.
Food is medicine. When your body gets the right fuel before surgery, recovery is often easier and faster.
How are Nutrition Needs Identified?
Your health care team may ask you a few simple questions to check if you could benefit from extra nutrition support before surgery.
What Can You Do Before Surgery?
Here are some important things to focus on:
- Eat three balanced meals every day that include a variety of foods. A simple way to ensure you are getting balanced meals is to use the Canada Food Guide plate model (see below).
- Try not to eat the same foods every day. Different foods have different nutrients. Choose foods you enjoy - this is an important part of healthy eating.
- Limit processed foods like packaged snacks, sugary drinks, and fast food.
- Reduce or avoid alcohol.

|
Protein Rich Foods (1/4 plate) |
- Help your body build muscle, heal wounds, fight infections, and regain strength for faster healing - Aim for 20-30 grams of protein at every meal (see graphic below for how much protein is in certain foods) - Eggs, meat, chicken, fish, milk, greek or regular yogurt, cheese, cottage cheese, nuts, seeds, soy foods, beans |
|
Vegetables and Fruits (1/2 plate) |
- Give your body the vitamins and minerals to stay strong and heal faster after surgery - Choose a range of colourful vegetables and fruits to get the vitamins, minerals, and antioxidants your body needs - Carrots, peppers, cucumber, celery, broccoli, cauliflower, leafy greens, squash, okra, pumpkin, sweet potato |
|
Whole Grains (1/4 plate) |
- Give your body steady energy to recover from surgery - Quinoa, rice, oats, barley, buckwheat, amaranth, millet, whole grain pasta, bread, crackers |
| Healthy Fats |
- Give your body energy for healing and recovery - Reduce swelling and inflammation - Olive oil, avocado oil, nuts, seeds, fatty fish, avocado |
| Water | - Keeps your body hydrated for faster healing and recovery |
How Much Protein Is In My Food?

If You Do Not Feel Hungry or Get Full Quickly
Try these tips:
- Eat protein first - Start with your protein foods before salad, fruit, or dessert so you get enough protein.
- Have smaller meals more often - Instead of 3 big meals, try 5-6 smaller meals or snacks throughout the day. Take snacks with you if you will be away from home.
- High protein snack ideas - Trail mix, greek yogurt with berries, hummus with vegetables, peanut butter on celery sticks with raisins, cheese and crackers, canned tuna and crackers, cottage cheese with fruit
- Choose drinks that give you energy - Milk, smoothies with protein powder, or nutrition shakes with extra protein, vitamins, and minerals
- Limit low-calorie drinks at mealtime - Coffee and tea can fill you up and make it harder to eat enough. Drink water between meals to stay hydrated.
Additional Nutrients to Support Healing
Omega-3 Fatty Acids
- Support muscle recovery and reduce swelling (inflammation)
- Found in salmon, mackerel, chia seeds, walnuts, flaxseeds
- Best to get from food instead of supplements before surgery because some omega-3 supplements can increase bleeding risk during surgery
Vitamin D
- Supports muscle strength and bone health, especially in older adults
- Found in fatty fish, fortified dairy, egg yolks, or supplements
Iron
- Maintains blood iron levels which lowers the chance of needing a blood transfusion
- Found in meat, fish, poultry, beans, peas, lentils, and some vegetables
Registered Dietitians
A dietitian can help you understand what your current diet may be missing and give you ideas to meet the guidance above. Many patients may benefit from a dietitian's support, especially if you:
- Have lost weight without trying or have noticed changes in your appetite
- Have health conditions like diabetes, kidney disease, or cancer
To contact a dietitian:
- You do not need a referral to see a dietitian.
- Contact a dietitian through HealthLinkBC by calling *811 or by email.
- Visit www.bcdietitians.ca to find a dietitian near you.
- Dietitian services are not covered by MSP, but are covered by many extended health benefits and insurance plans.
Fasting Before Surgery
Your health care team will give you clear instructions for when to stop eating and drinking before surgery. Following the instructions is very important to keep you safe and prevent your surgery from being delayed. Do NOT fast for longer than your team tells you - your body heals best when it has enough fuel.
Preparing for After Surgery
After surgery you may feel tired and have less energy or mobility to cook. Planning ahead, like making and freezing healthy meals, can make recovery easier. Here are some freezer-friendly meal ideas:
- Protein packed soups or stews with chicken, beef, lentils, or beans
- Casseroles or baked dishes with meat, tofu, or beans and vegetables
- Egg muffins or frittata are easy to grab breakfasts or snacks
- Frozen smoothie packs - fruit + leafy greens + protein powder
Where to Learn More
Healthlink BC - or call/text *811 to speak to a dietitian
BCdietitians.ca - find a dietitian near you
Food Banks BC - find local food banks for groceries and other essentials
bc.211.ca - or call *211 to find local food banks and supports
Obesity & Surgery: What You Need to Know
When your health care team talks with you about your weight before surgery, the goal is to keep you as safe and health as possible during and after your operation. These conversations are meant to support you, not to judge you.
Just like we talk about heart health with people who have heart problems, we talk about how weight may affect anesthesia (the medicine that puts you to sleep), healing, and recovery from surgery.
Every patient - no matter their body size - deserves respectful, high-quality care. Talking about these health factors like weight helps your care team give you the best support.
Why Does Weight Matter Before Surgery?
Carrying excess body weight can increase the risk of complications during and after surgery such as breathing or heart issues, blood clots, wound infections, slower healing, and longer hospital stays. Not everyone experiences these complications, but as BMI increases, the chances of certain risks may increase.
To reduce your surgical risk, your health care team may:
- Screen for conditions like sleep apnea, diabetes, or heart problems
- Refer you to an anesthesiologist for extra planning
- Suggest seeing a sleep specialist or obesity medicine specialist
This helps your health care team create a personal plan for anesthesia, pain control, and recovery.
How is Obesity Identified?
Doctors often use Body Mass Index (BMI), which compares weight to height, to help identify potential health factors before surgery. BMI can be helpful, but it does not tell the whole story because it does not consider:
- Muscle mass and bone structure
- Ethnicity
- Other health conditions like high blood pressure, insulin resistance, or diabetes.
This is why your health care team looks at other health measures like waist size, diabetes, heart health, sleep problems, strength, mobility (your ability to move around), and daily function.
What Can You Do Before Surgery?
You can do a lot to make surgery safer and recovery faster:
- Ask questions - Your health care team is here to help, not judge.
- Share your goals - Whether it is feeling stronger, sleeping better, or managing health conditions like diabetes, your health care team wants to support you.
- Share your challenges - If time, mobility, or money make things difficult, your health care team can connect you with helpful resources.
- Stay active - Even small amounts of movement can make your lungs, heart, and muscles stronger for surgery and recovery (Refer to the Getting Active section for more information).
- Eat balance meals - Balanced meals with more protein and vegetables and less added sugar help your body heal. Drink plenty of water to stay hydrated (Refer to the Nutrition section for more information).
- Follow through with referrals - Specialists are part of your plan to support your safety.
We know conversations about weight can be hard. Your health care team is committed to:
- Respecting every body
- Looking at your whole health, not just weight
- Helping you prepare for surgery in a way that feels empowering and supportive
Where to Learn More
Learn more about healthy weight, healthy eating, and physical activity at Healthlink BC or Obesity Canada
Quitting Smoking Before Surgery: What You Need to Know
Smoking affects how your body heals. Cutting down or quitting smoking before surgery can help you heal faster and lower your chance of having problems during and after surgery.
The sooner you quit, the better your body will heal. By quitting or cutting back now, you can:
- Lower your risk of pnuemonia (lung infection)
- Reduce your chance of a heart attack
- Help your incision heal faster and reduce your risk of infection
How is Smoking Risk Identified?
If you smoke or use electronic cigarettes (vaping), it is important to know that smoking can increase the risk of problems during and after surgery.
Your health care team may talk with you about this at different times. You may hear it from your surgeon, anesthesiologist, nurse, or pharmacist. This is not meant to judge you. The goal is to make sure everyone who wants help can get the right support.
We want to clearly explain the risks so you can make informed decisions. Even small steps, like cutting back, can make a big difference in your recovery.
What Can You Do Before Surgery?
Quitting is not just about willpower. Nicotine is addictive and your body may need help to get through withdrawal. It can take time to achieve success. Talk to your pharmacist for recommendations on products and to build a plan to quit before surgery.
Successful quit plans often include:
- Nicotine replacement therapies (NRT) like gum, patches, lozenges, or sprays
- Prescription medication (like varenicline or bupropion)
These treatments reduce cravings and other uncomfortable withdrawal symptoms. They have been shown to double or even triple the chance of success. These can be prescribed by your family doctor, nurse practitioner, or pharmacist - and they may be fully covered by Pharmacare.
BC PharmaCare's Smoking Cessation Program
Helps eligible BC residents stop using tobacco products by paying for:
- The full cost of nicotine gum, lozenges, and patches, or sprays
- Some or all of the cost of certain smoking cessation prescription drugs, with coverage depending on your PharmaCare plan
Other Benefits of Quitting Smoking
- Add 6-8 more years to your life
- Save up to $3,000 per year
- Lower your risk of cancer, lung diseases, and heart disease
- Protect your loved ones from secondhand smoke
Where to Learn More
Learn more about quitting smoking at Healthlink BC
Access telephone support for smoking cessation at *211
Quit Now is a free quit smoking program delivered by the BC Lung Association that offers free 1:1 coaching, peer support groups, and resources to help you cut back or quit completely.
First Nations Health Authority - Respecting Tobacco
Sleep Apnea & Surgery: What You Need to Know
Obstructive sleep apnea (OSA) is when someone's breathing stops or gets very shallow during sleep. This happens because their airway gets blocked when the muscles in the head and neck relax. Many people with OSA do not know they have it.
Sleep apnea can be treated and managing it before and after surgery makes surgery safer and helps you recover faster.
If you have sleep apnea, getting treatment can:
- Prevent serious health problems over time such as stroke, heart disease, high blood pressure, diabetes, and kidney problems
- Prevent daytime sleepiness, which can increase the risk of car accidents or injuries
- Decrease the risk of breathing problems while under anesthesia (the medicine that puts you to sleep for surgery)
- Increase your oxygen levels
- Prevent abnormal heart rhythms and heart attacks
- Shorten your hospital stay and reduce complications during recovery
How is Sleep Apnea Found?
Your health care team will ask you some questions to see if you may have sleep apnea. If they think you may have sleep apnea, a sleep study may be done to check your breathing, heart rate, and oxygen while you sleep. This can be done at home or in a lab.
Talk to your health care team if:
- You snore loudly, gasp, or stop breathing at night
- You feel very tired or sleepy during the day
- You were told you might have sleep apnea but have not been tested yet
- Your CPAP or other treatment is uncomfortable or you have stopped using it
What Can You Do Before Surgery?
If You Have Sleep Apnea
- Keep using your treatment device (CPAP, BPAP, or mouthguard) every night, including the nights before and after surgery
- Bring your machine to the hospital, even for day surgery
- Talk to your health care team if you have stopped using your treatment
- Ask your primary care provider to send your sleep study results to your surgical team
If Your Health Care Team Thinks You May Have Sleep Apnea
- Your health care team may suggest a Home Sleep Apnea Test (HSAT) or a sleep study in a lab
- Your health care team may suggest starting treatment (CPAP) prior to your surgery
How To Stay Safe After Surgery
These tips apply whether you have a sleep apnea diagnosis or are waiting for testing:
- Use your prescribed treatment (e.g., CPAP) every time you nap or sleep for the first week after surgery
- Avoid sleeping flat on your back - sleep on your side or with your shoulders slightly raised with pillows
- Avoid alcohol, cannabis, and sedating medications unless your health care team says it is okay
- Use the lowest dose of pain medication you can. Non-sedating options like acetaminophen (Tylenol) or ibuprofen are often safer
- Talk to your health care team about other pain control options like nerve blocks or epidurals to reduce your need for sedating medications
- Your health care team will watch your breathing carefully. You may need extra observation or to stay in the hospital overnight
Where To Learn More
Learn more about sleep apnea at Healthlink BC
Substance Use & Surgery: What You Need to Know
Substances like recreational or illicit drugs, even if used only once in a while, can change how your body reacts to anesthesia and pain mediation. If your health care team knows what drugs you have used and how often, they can create a plan that helps keep you safe and comfortable before, during, and after your procedure.
Avoiding substance (drug) use before surgery may:
- Make anesthesia safer
- Decrease your risk of infection and speed up healing
- Lead to shorter hospital stays and prevent complications
Discussing your substance use with your health care team helps them plan safe anesthesia, effective pain control, withdrawal prevention and a smoother transition from hospital to home.
How is Substance Use Identified?
As part of your pre-surgical screening, we ask if you have used any non-prescribed substances (like street drugs, party drugs, or stimulants) in the past 12 months. If you said yes, we may ask more questions about the type, amount, and how often you use - this is only to make your care safer. Your answers are confidential and are used only as part of your health history.
Even if you used a substance just once in the last 12 months, we are sharing this information so you can make informed decisions and understand how it may affect your surgical care. This information supports conversations with your health care team, but does not replace them.
What Can You Do Before Surgery?
If you use non-prescribed substances (drugs):
- Try to reduce or pause use for at least 48 hours before surgery (longer is better). This reduces your risk of complications.
- If you use substances daily or most days, talk with your health care team. It may be safest to slowly reduce your dose to avoid withdrawal.
- Do not come to surgery intoxicated. If you are visibly high on the day of surgery, your surgery may be rescheduled for your safety.
- Stimulants like cocaine or methampehtamine carry high risks. Avoid them for at least 2 weeks before surgery. The longer you can avoid them before surgery, the safer you will be.
- Talk to your health care team for help planning your care.
Are You On Opioid Agonist Therapy (OAT)?
If you take methadone, Suboxone, or Kadian, here is what you need to know:
- Usually you should keep taking your medication as prescribed, including the day of surgery (in some cases your health care team may change your dose before surgery but they will let you know).
- Meet with your community prescriber before surgery to review your dose and make a plan for after surgery.
- If you are admitted early in the morning, arrange a "carry" dose so you do not miss your medication
If you take Naltrexone or Contrave, you may need special instructions. Ask your health care team about when to stop and restart these medications.
If You Want to Cut Back or Quit
If you use substances daily or in large amounts, stopping suddenly can cause withdrawal symptoms. Sometimes withdrawal can be dangerous, which is why a slow, supported taper is often recommended. This helps keep you safe while reducing your use.
If needed, your health care team may refer you to:
- An Addiction Medicine specialist
- Your primary care provider
- Community support services to help create a safer plan
Prevent Overdose - Protect Yourself and Others
Because some drugs may be contaminated with dangerous substances like fentanyl, it is important to:
- Pick up a free naloxone kit from your local pharmacy
- Learn how to recognize and respond to an overdose. Visit the BC Government website to learn more.
Where to Learn More
Learn more about mental health and substance use at HealthLinkBC
Visit Help Starts Here for substance use support and resources
First Nations Health Authority Information About Opioid Agonist Therapy
24-Hour BC Alcohol and Drug Info Line: 1-800-663-1441
Support After Surgery: What You Need to Know
After surgery, your body needs time to rest, heal, and regain strength. Having support at home can make your recovery smoother, safer, and help you avoid complications or delays in leaving the hospital.
The amount of help you will need depends on the type of surgery you are having. For many procedures - especially same-day (daycare) surgeries - you must have a responsible adult to take you home. This person should:
- Help you get home safely
- Assist with daily tasks
- Watch for any signs that something might by wrong
Who Needs Support After Surgery?
During your pre-surgical screening, you may be asked:
- Do you have a responsible adult who can help you during your recovery?
- Do you have a responsible adult who can take over caregiving responsibilities (like caring for children, pets, or vulnerable adults)?
These plans must be in place before your surgery day to ensure a safe discharge home. If you answered no to either of these questions, we will follow-up to ensure you are prepared for surgery.
What Can You Do Before Surgery?
Traditional criteria for discharge after day surgery includes having a responsible adult to take you home. Here are some important things to organize ahead of time:
- Line up a support person to:
- Drive you home from the hospital (or come with you in a taxi/uber)
- Stay with you overnight (or longer, if needed)
- Help with meals, mobility (walking or moving), medications, and/or personal care
- Ask your health care team:
- How long will I be in the hospital?
- Will I have any movement limitations (like needing crutches or a walker)?
- What medications will I need to pick up?
- What should I expect for my recovery? When will I be back to my usual activities?
Where to Learn More
There are options available to help you get the care you need:
- Visit the BC Government website or call *211 for information on how to arrange for home care if a capable adult is not available.
- Research private home care companies if you prefer to arrange your own help
- Ask your surgical team to connect you with a hospital social worker
Voicing What Matters Most: What You Need to Know
Before your surgery, it is important to take some time to think about what matters most to you and the kind of care you would want if a serious emergency happened while you are in the hospital. This includes the kind of care, treatments, and ways of living that you would or would not want.
Sometimes you may not be able to speak for yourself. Writing down your wishes helps your health care team and loved ones understand what is most important to you. This way, your care matches your values. Clear wishes can also guide your loved ones and give them comfort when making decisions on your behalf.
These conversations are not meant to scare you. They are meant to help in several ways:
- Make sure your care matches your values and wishes.
- Make sure that surgery is right for you.
- Reduce stress for you and your loved ones by thinking ahead.
- Let your health care team know your preferences if you cannot speak for yourself (for example, if you are under anesthetic or too ill to speak).
Who Needs to Talk About Goals of Care?
Your health care team might ask about what is important to you, what you want your life to look like after surgery, and what kinds of care you would or would not want. This may be called a "goals of care" conversation. These conversations are normal and routine before surgery.
They are especially common when:
- You do not have a written advance care plan or substitute decision maker
- You are having major surgery
- You are older, frail, or have multiple health conditions
If your health care team does not start this conversation with you, you can share your advance care plan or tell them what matters most to you.
What Can You Do Before Surgery?
Here are a few steps you can take now:
- Think about what matters most for your health and happiness
- Choose someone you trust to speak for you if you cannot. This is called a substitute decision-maker.
- Write down what is important to you and the types of treatment you would or would not want. The following tools can help with this:
- Share what you wrote with your substitute decision maker and/or your loved ones so they know your wishes.
Be Prepared for a MOST Conversation
Before surgery, your doctor (often your surgeon or anesthesiologist) will complete a Medical Orders for Scope of Treatment (MOST). This order tells the health care team what treatments you want if your health gets worse during or after surgery.
Some treatments included in a MOST order are::
- CPR (chest compressions or electric shocks to your heart)
- Being on a breathing machine beyond surgery
Your MOST order can be updated at anytime if your health or wishes change. It will always reflect the most recent conversation.
The graphic and video linked below can help you make decisions about Cardiopulmonary Resuscitation (CPR).
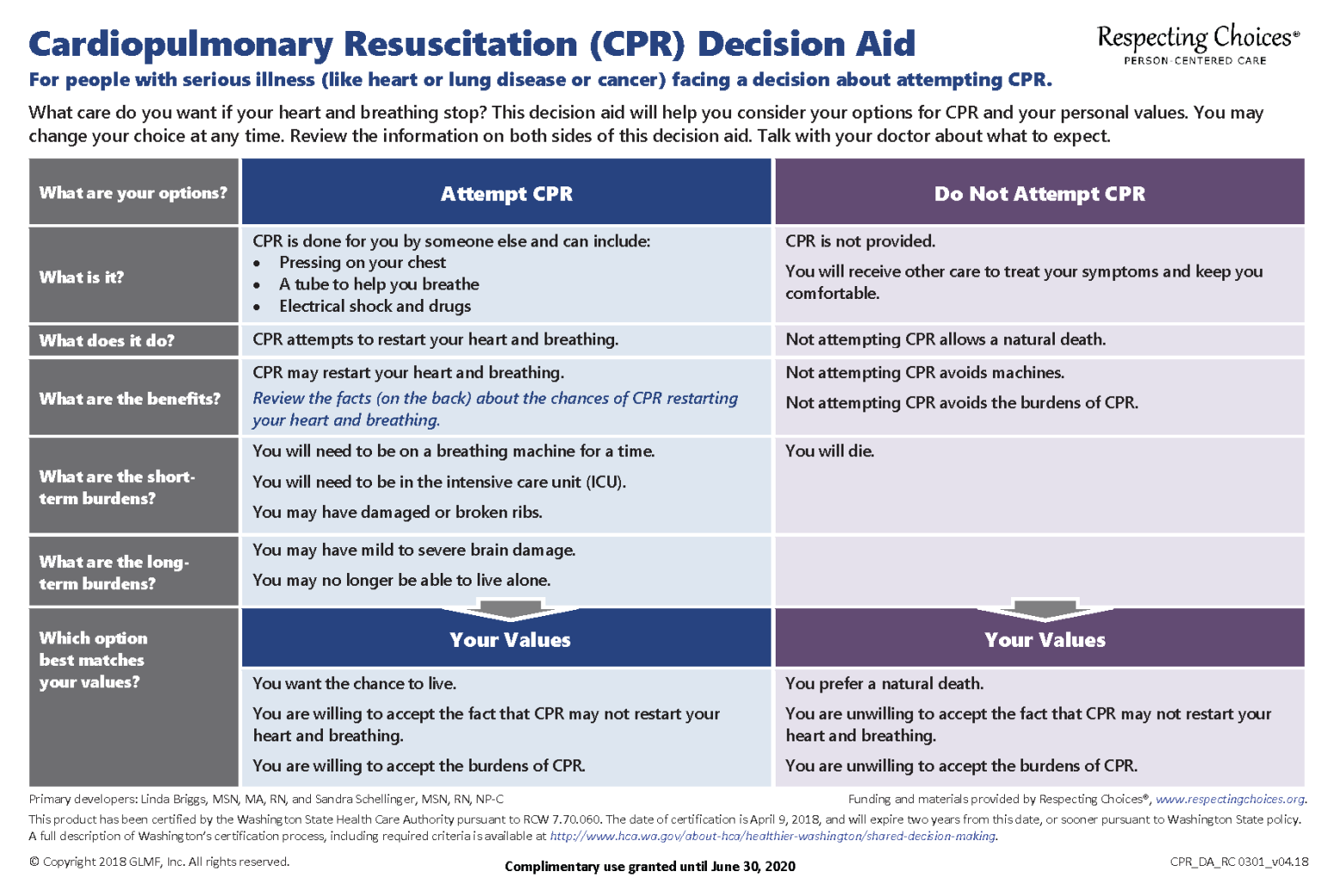
Watch this Video on Preparing Patients and Their Families for Shared Decision-Making About Cardio-Pulmonary Resuscitation
