Obesity
Obesity is linked to several conditions, such as type II diabetes and obstructive sleep apnea, that may increase perioperative risks. Comorbidities may outweigh BMI in assessing these risks. (1-4)
For patients with class 1* obesity (BMI: 30–34.9), perioperative risks are mainly limited to venous thromboembolism. In class 2* obesity (BMI: 35–39.9) and higher, there is a modest increase in risks, including postoperative pulmonary complications, wound infections, longer hospital stays, increased blood loss, longer surgeries, and renal failure. (5-8)
Although high BMI is associated with higher perioperative risks, there is limited research on the effects of preoperative weight loss through diet and limited evidence to suggest delaying surgery based on BMI. (9)
*Classification is based on Caucasian populations. Lower cutoffs have been recommended for other ethnicities. (10)
Screening Tools
Although BMI is easy to obtain and therefore used to identify and categorize severity of obesity, integrating other indices (e.g., waist to hip ratio, waist circumference, and percent body fat) may improve predictions of metabolic health, comorbid conditions, and perioperative risk stratification. (1-3)
Prehabilitation and Optimization Algorithm
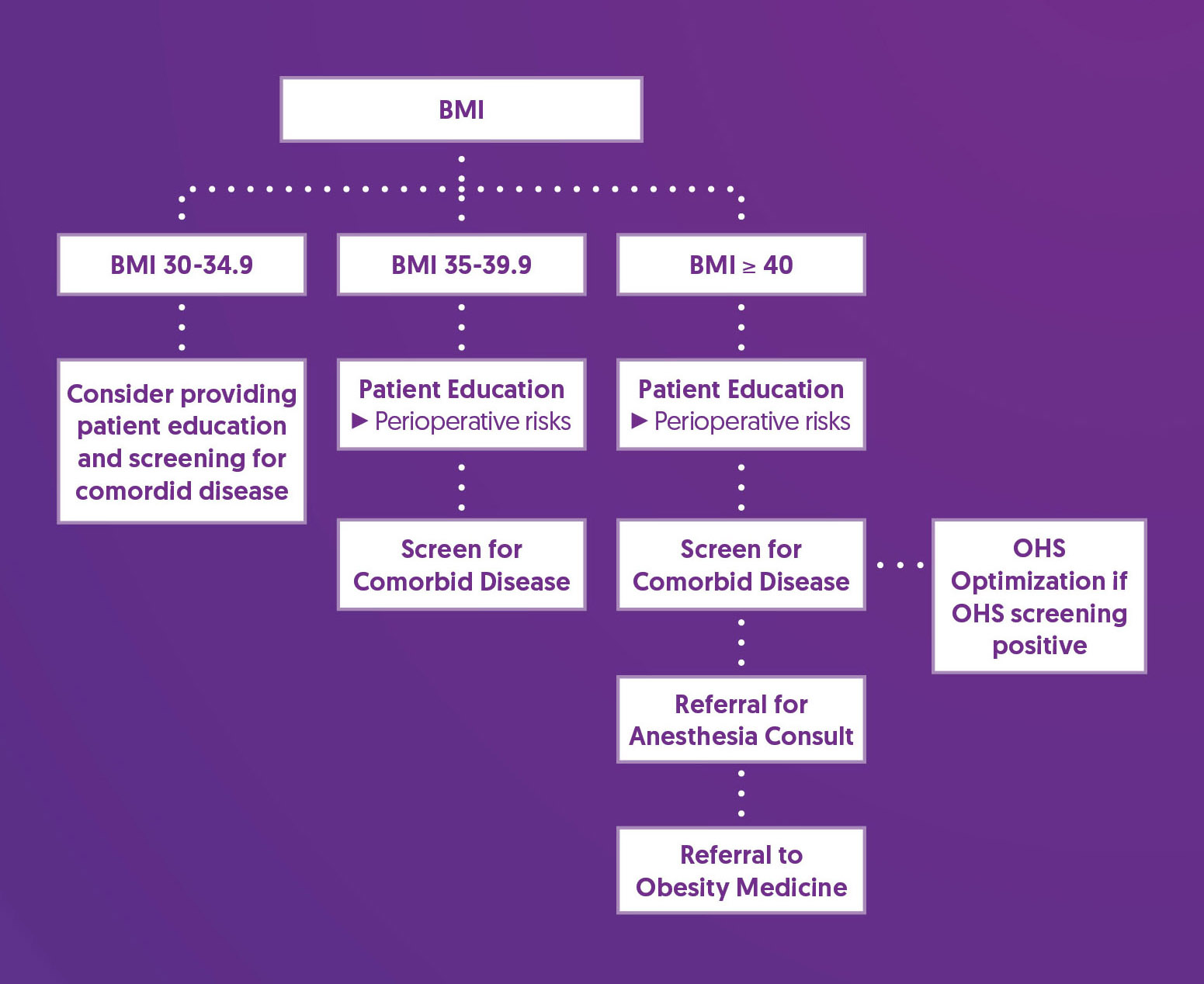
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Screen for Comorbid Disease |
|
| Obesity Hypoventilation Syndrome (OHS) |
|
| Referral for Anesthesia Consult |
|
| Consider Referral to Obesity Medicine |
|
References
1. Wharton, S., Lau, D. C. W., Vallis, M., Sharma, A. M., Biertho, L., Campbell-Scherer, D., Adamo, K., Alberga, A., Bell, R., Boulé, N., Boyling, E., Brown, J., Calam, B., Clarke, C., Crowshoe, L., Divalentino, D., Forhan, M., Freedhoff, Y., Gagner, M., Glazer, S., … Wicklum, S. (2020). Obesity in adults: a clinical practice guideline. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 192(31), E875–E891. https://doi.org/10.1503/cmaj.191707
2. Gurunathan, U., & Myles, P. S. (2016). Limitations of body mass index as an obesity measure of perioperative risk. British journal of anaesthesia, 116(3), 319–321. https://doi.org/10.1093/bja/aev541
3. Ledford, C. K., Ruberte Thiele, R. A., Appleton, J. S., Jr, Butler, R. J., Wellman, S. S., Attarian, D. E., Queen, R. M., & Bolognesi, M. P. (2014). Percent body fat more associated with perioperative risks after total joint arthroplasty than body mass index. The Journal of arthroplasty, 29(9 Suppl), 150–154. https://doi.org/10.1016/j.arth.2013.12.036
4. Chan, W. K., Chuah, K. H., Rajaram, R. B., Lim, L. L., Ratnasingam, J., & Vethakkan, S. R. (2023). Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review. Journal of obesity & metabolic syndrome, 32(3), 197–213. https://doi.org/10.7570/jomes23052
5. Dindo, D., Muller, M. K., Weber, M., & Clavien, P. A. (2003). Obesity in general elective surgery. Lancet (London, England), 361(9374), 2032–2035. https://doi.org/10.1016/S0140-6736(03)13640-9
6. De Oliveira, G. S., Jr, McCarthy, R. J., Davignon, K., Chen, H., Panaro, H., & Cioffi, W. G. (2017). Predictors of 30-Day Pulmonary Complications after Outpatient Surgery: Relative Importance of Body Mass Index Weight Classifications in Risk Assessment. Journal of the American College of Surgeons, 225(2), 312–323.e7. https://doi.org/10.1016/j.jamcollsurg.2017.04.013
7. Madsen, H. J., Gillette, R. A., Colborn, K. L., Henderson, W. G., Dyas, A. R., Bronsert, M. R., Lambert-Kerzner, A., & Meguid, R. A. (2023). The association between obesity and postoperative outcomes in a broad surgical population: A 7-year American College of Surgeons National Surgical Quality Improvement analysis. Surgery, 173(5), 1213–1219. https://doi.org/10.1016/j.surg.2023.02.001
8. Kassahun, W. T., Mehdorn, M., & Babel, J. (2022). The impact of obesity on surgical outcomes in patients undergoing emergency laparotomy for high-risk abdominal emergencies. BMC surgery, 22(1), 15. https://doi.org/10.1186/s12893-022-01466-6
9. Pavlovic, N., Boland, R. A., Brady, B., Genel, F., Harris, I. A., Flood, V. M., & Naylor, J. M. (2021). Effect of weight-loss diets prior to elective surgery on postoperative outcomes in obesity: A systematic review and meta-analysis. Clinical obesity, 11(6), e12485. https://doi.org/10.1111/cob.12485
10. Li, Z., Daniel, S., Fujioka, K., & Umashanker, D. (2023). Obesity among Asian American people in the United States: A review. Obesity (Silver Spring, Md.), 31(2), 316–328. https://doi.org/10.1002/oby.23639
11. Chau, E. H., Lam, D., Wong, J., Mokhlesi, B., & Chung, F. (2012). Obesity hypoventilation syndrome: a review of epidemiology, pathophysiology, and perioperative considerations. Anesthesiology, 117(1), 188–205. https://doi.org/10.1097/ALN.0b013e31825add60