Pain Management
Significant acute postoperative pain is common, even among those on an established pain management protocol (1). Pain after surgery is associated with increased risk of postoperative readmission to hospital, emergency department visits, myocardial injury, delirium, and chronic pain (2-7). Postoperative pain control may be improved by addressing modifiable patient risk factors such as sleep, BMI, depression, anxiety, and preoperative pain (8).
Screening Tools
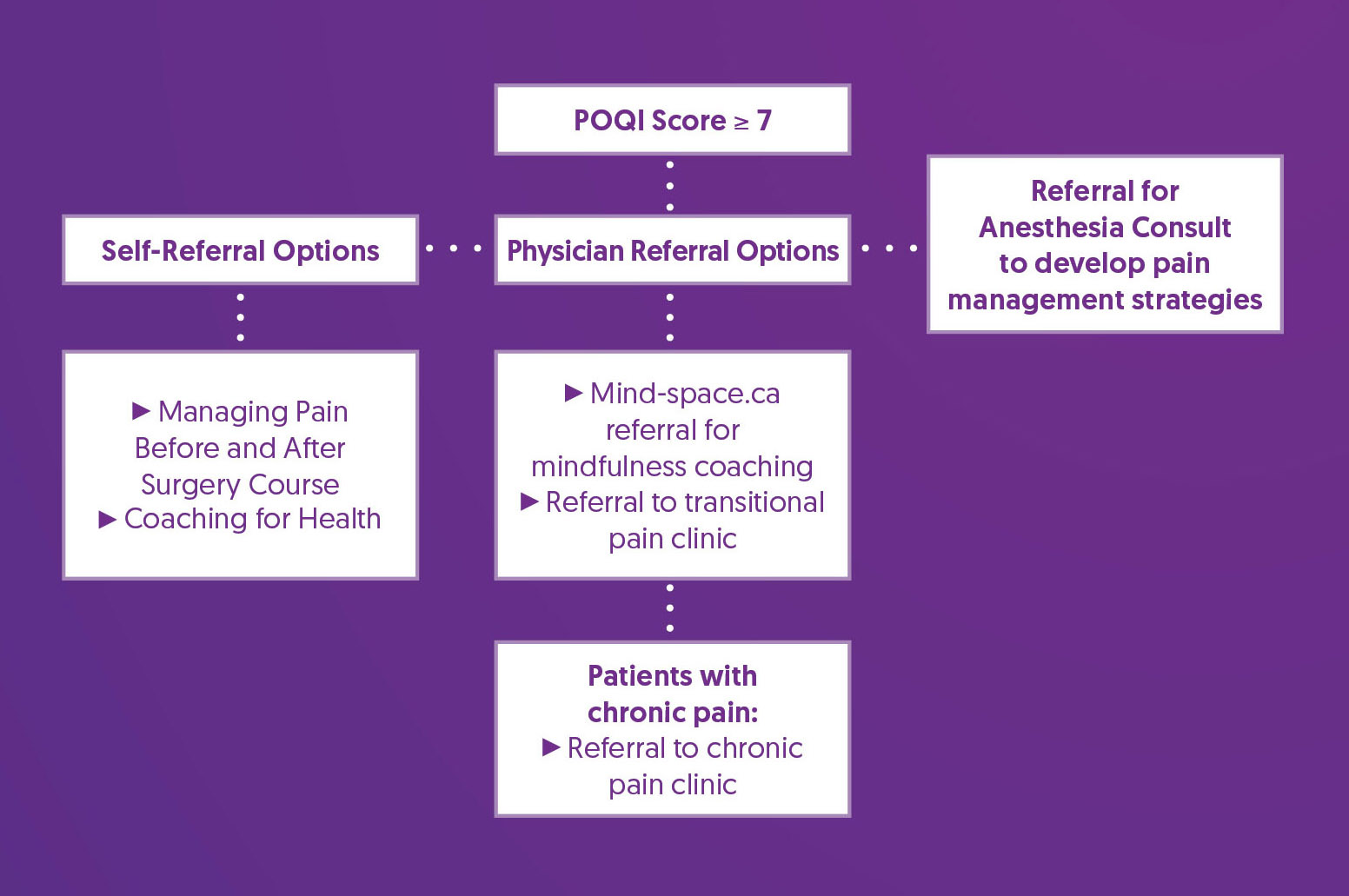
The Perioperative Opioid Quality Improvement (POQI) score is an algorithm being developed at St. Paul's Hospital. It aims to identify patients at increased risk of significant postoperative pain and long-term opioid use, so that their care plans may be tailored with the intent of helping reduce initial opioid consumption. (9) It incorporates several variables associated with increased risk for developing postoperative pain and uses consumption of > 90 morphine milligram equivalents per day while inpatient after surgery as a surrogate marker for assessing performance (9). While the POQI score is not validated, it was selected to support postoperative pain risk stratification based on local BC experience with the tool. A POQI score >= 7 is considered to be ‘increased risk.’
Perioperative Opioid Quality Improvement (POQI) Assessment

Prehabilitation and Optimization Algorithm
Prehabilitation and Optimization Recommendations
| Patient Education |
|
| Self-Referral Options |
|
| Referral for Anesthesia Consult |
|
| Physician-Referral Options |
|
References
1. Sommer, M., de Rijke, J. M., van Kleef, M., Kessels, A. G., Peters, M. L., Geurts, J. W., Gramke, H. F., & Marcus, M. A. (2008). The prevalence of postoperative pain in a sample of 1490 surgical inpatients. European journal of anaesthesiology, 25(4), 267–274. https://doi.org/10.1017/S0265021507003031
2. Katz, J., Jackson, M., Kavanagh, B. P., & Sandler, A. N. (1996). Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. The Clinical journal of pain, 12(1), 50–55. https://doi.org/10.1097/00002508-199603000-00009
3. Hernandez-Boussard, T., Graham, L. A., Desai, K., Wahl, T. S., Aucoin, E., Richman, J. S., Morris, M. S., Itani, K. M., Telford, G. L., & Hawn, M. T. (2017). The fifth vital sign: Postoperative pain predicts 30-day readmissions and subsequent emergency department visits. Annals of Surgery, 266(3), 516–524. https://doi.org/10.1097/SLA.0000000000002372
4. Dubljanin Raspopović, E., Meissner, W., Zaslansky, R., Kadija, M., Tomanović Vujadinović, S., & Tulić, G. (2021). Associations between early postoperative pain outcome measures and late functional outcomes in patients after knee arthroplasty. PLOS ONE, 16(7), e0253147. https://doi.org/10.1371/journal.pone.0253147
5. Buvanendran, A., Della Valle, C. J., Kroin, J. S., Shah, M., Moric, M., Tuman, K. J., & McCarthy, R. J. (2019). Acute postoperative pain is an independent predictor of chronic postsurgical pain following total knee arthroplasty at 6 months: A prospective cohort study. Regional Anesthesia & Pain Medicine, 44(3), e100036. https://doi.org/10.1136/rapm-2018-100036
6. Turan, A., Leung, S., Bajracharya, G. R., Babazade, R., Barnes, T., Schacham, Y. N., Mao, G., Zimmerman, N., Ruetzler, K., Maheshwari, K., Esa, W. A. S., & Sessler, D. I. (2020). Acute Postoperative Pain Is Associated With Myocardial Injury After Noncardiac Surgery. Anesthesia & Analgesia, 131(3), 822–829. https://doi.org/10.1213/ANE.0000000000005033
7. Khaled, M., Sabac, D., Fuda, M., Koubaesh, C., Gallab, J., Qu, M., Lo Bianco, G., Shanthanna, H., Paul, J., Thabane, L., & Marcucci, M. (2024). Postoperative pain and neurocognitive outcomes after noncardiac surgery: a systematic review and dose-response meta-analysis. British journal of anaesthesia, S0007-0912(24)00550-6. Advance online publication. https://doi.org/10.1016/j.bja.2024.08.032
8. Yang, M. M. H., Hartley, R. L., Leung, A. A., Ronksley, P. E., Jetté, N., Casha, S., & Riva-Cambrin, J. (2019). Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ open,9(4), e025091. https://doi.org/10.1136/bmjopen-2018-025091
9. Görges, M., Sujan, J., West, N. C., Sreepada, R. S., Wood, M. D., Payne, B. A., Shetty, S., Gelinas, J. P., & Sutherland, A. M. (2024). Postsurgical Pain Risk Stratification to Enhance Pain Management Workflow in Adult Patients: Design, Implementation, and Pilot Evaluation. JMIR perioperative medicine, 7, e54926. https://doi.org/10.2196/54926